Scientists are hoping advances in cancer research could lead to a day when a patient’s own immune system could be used to fight and destroy a wide range of tumors.
Cancer immunotherapy has some remarkable successes, but its effectiveness has been limited to a relatively small handful of cancers. In APL Bioengineering, a team from Stanford University and Genentech describes how advances in engineering models of tumors can greatly expand cancer immunotherapy’s effectiveness to a wider range of cancers.
“One of the biggest breakthroughs we’ve had in cancer research in decades is that we can modify the cells in your own immune system to make them kill cancer cells,” said author Joanna Lee.
Using existing immunotherapy advances, scientists have figured out a way to make the T-cells already inside ‘hot’ or inflamed tumors start fighting them. But that breakthrough does not help with ‘cold’ or noninflamed tumors, because the immune cells are not in the right place.
“Now, a big push in drug discovery in cancer is how do how to make those cold tumors hot?” Lee said. “How do we get immune cells into those tumors?”
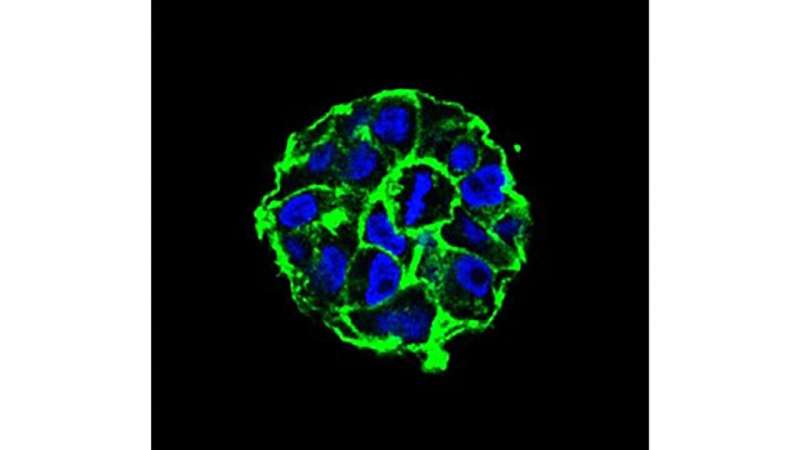
To do that, scientists need to first recreate those changes in a laboratory. While much research can be done in a 2-D environment, like a petri dish, modeling the way immune cells interact with cancer requires a more advanced 3-D environment.
Building the tumor microenvironment, Lee said, will require expertise from both biologists, like herself, and engineers, like co-author Ovijit Chaudhuri.
“Trying to merge those two fields together is what has made the 3-D culture field really challenging,” she said. “The reason it’s so hard is we are not just talking about having a plate you throw some cells in. It is more like building a house.”
A faithful 3-D model for cold tumors would make the research leading to new cancer drugs faster and more efficient. Lee said that is a big deal in a field where proposed new treatments take years to be approved and an overwhelming 96.6 % of them fail.
Source: Read Full Article
