Coronary artery disease (CAD) is the most common form of heart disease and is present in about 18.2 million American adults. This disease is defined by narrowing of the vessels that supply the heart with critical oxygen and nutrients, typically caused by plaque blockages and inflammation. But not all plaques have the same composition, and while blockages in the heart vessels can cause heart attacks and cardiac arrest, not all areas with blockage create problems with blood flow.
A recent study published in the International Journal of Cardiology examined a noninvasive method to predict which blockages require surgical intervention (stent placement or bypass surgery) and which can be treated without surgery. With the help of a multinational research team, Medical University of South Carolina researchers Akos Varga-Szemes, M.D., Ph.D., and U. Joseph Schoepf, M.D., performed a validation study with a novel artificial intelligence (AI) program to compare predictions made by the software to previously logged patient measurements.
The baseline measurements were determined by the currently accepted care standard, which requires catheterization to check the flow rate inside vessels. With the new program, Schoepf and Varga-Szemes aim to characterize the blood flow in the heart vessels noninvasively to decide which patients are good candidates for having their vessels reopened and those better left alone.
The study analyzed data from 113 patients with suspected CAD who had undergone noninvasive coronary CT scanning as well as invasive catheterization to measure blood flow, specifically a number called the fractional flow reserve (FFR). For coronary CT scanning, patients received a dye injection for imaging of the coronary blood vessels. For catheterization, a catheter with a pressure sensor was inserted through a vessel in the arm or leg and steered to the heart and the target blockage, a procedure that carries all of the discomfort and many of the risks of invasive surgery.
The compiled data set was used as the standard baseline, and the researchers deployed the AI software to make its predictions based on CT data for the three major coronary arteries (left anterior descending artery, left circumflex artery and right coronary artery) and the branching arteries. They then compared the data sets to determine the software’s prediction accuracy.
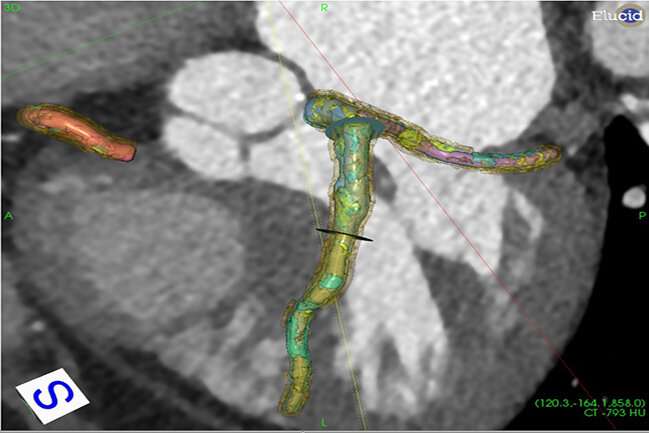
The team used the commercially available software vascuCAP, a system based on AI that they are developing with the biotech company Elucid. The software looks at coronary CT images of the heart vessels and plaques and determines the makeup of the plaques. This information itself can be useful to clinicians because the composition of a plaque influences the elasticity of vessels and the risk of altered blood flow—for example, fatty plaques with a lot of lipids are more fragile and more likely to eventually lead to a heart attack, whereas plaques made up of calcium are more stable and less likely to be associated with a heart attack. And importantly, the software’s AI algorithms then use the plaque composition to estimate the blood flow through that region.
“What we are talking about is an artificial intelligence algorithm which learns the different characteristics or different components of the blockage,” Varga-Szemes said. “Based on those results, it predicts whether this limits the blood flow.”
The algorithm calculates the FFR by estimating the flow rates upstream and downstream of the plaque and determining the difference. While this is the same measurement performed by catheterization, a catheter is a stiff instrument which needs to be forced through the vessels to reach to and beyond plaques. But because plaques are often fragile and unstable and the procedure itself has some risk of complications, avoiding this risk is preferable if possible.
Furthermore, the software can examine the blood flow through multiple target areas and slide up and down a vessel without the manipulation that would be required with catheterization. It also provides clinicians a map of the entire cardiac vessel network, revealing any areas of concern and providing numeric values to indicate the flow rates.
The results of the validation study showed that the software worked well and provided results that correlated very closely with the results obtained by catheterization, but without the risks of an invasive procedure and at a fraction of the time and cost.
The potential to predict the significance of CAD blockages noninvasively is great news for patients, who may be able to avoid the discomfort and risks of invasive catheterization while still minimizing their cardiac risks and receiving the treatment they need. It also benefits clinicians and hospitals by saving valuable catheter suite time and costs while still providing the information physicians need to choose the best treatment plans for their patients.
“There are high-risk features that can be seen on CT that help us to predict which patients are more prone to have a heart attack in the future, regardless of what the blood flow looks like at the time,” Schoepf said. “So physicians can identify which patients need their help right now but also which patients need more TLC in their treatment to prevent heart attacks further down the road.”
Source: Read Full Article
