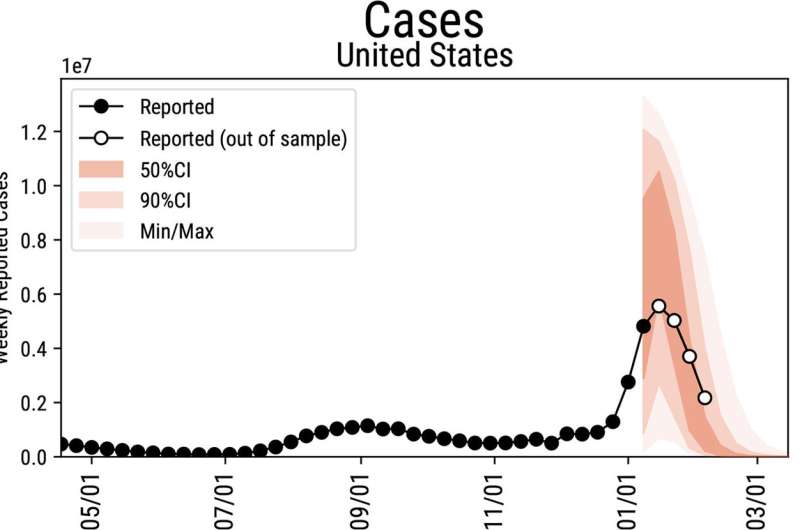
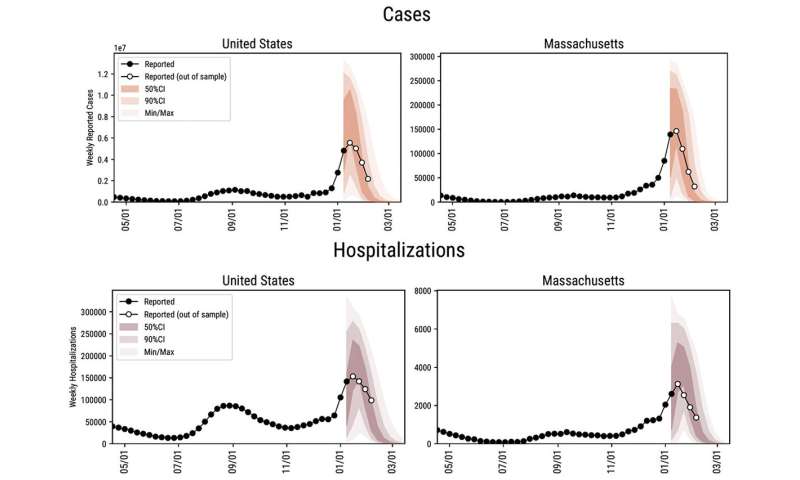
The crest of the omicron wave is in the rearview mirror in the United States. Daily new COVID-19 cases have fallen to half those of the peak of the surge in mid-January. Hospitalizations—a metric that lags behind new case counts—also are declining significantly across the country.
“What we have for the next few weeks should be a decrease in activity. All of the indicators seem to go down,” says Alessandro Vespignani, director of the Network Science Institute and Sternberg Family Distinguished Professor at Northeastern. Vespignani leads a team of infectious-disease modelers that has been developing a set of projections about the possible futures of the COVID-19 pandemic since the crisis began.
If there are no surprises, Vespignani’s team projects that COVID-19 case rates should return to pre-omicron levels in March. And by late spring or early summer, he says, the U.S. and other countries in the Northern Hemisphere may be able to breathe a little easier.
“We might have a considerable break from COVID-19” during the warmer months, Vespignani says. “We will spend more time outside, and the virus doesn’t like the sun and the warmer temperatures.”
But that is not a certain future, and trouble could still arise before then, he says. As the emergence of the omicron variant showed, highly transmissible mutations in SARS-CoV-2, the coronavirus that causes COVID-19, can change the trajectory of the pandemic quickly.
“Likely there will be other bumps in the road,” Vespignani says. But “what we think is plausible is that those bumps will be less threatening.”
Pandemic-watchers have been keeping an eye on a mutated version of the omicron variant that has begun to circulate in some places, particularly in parts of Europe and Asia. Nicknamed “omicron 2” or sometimes “stealth” omicron, the variant that virologists call BA.2 seems to be quite similar to the original omicron variant (BA.1), with just a few mutations.
“This could create some bumps in the next few weeks,” Vespignani says. But he does not expect there to be major surges in COVID-19 cases as a result of BA.2.
As for other concerning variants that might emerge this spring, “We don’t have a crystal ball,” Vespignani says. “We must hope there will be no surprises.”
The biggest bumps may come in the fall or winter months of 2022. That’s typically when respiratory illnesses such as the flu rise—and that pattern has been emerging in the coronavirus cases, too.
“What happens next winter will depend a lot on what kind of mutation the virus will have, which strain will be circulating, the level of vaccination in the population, and the duration of the immunity provided by the omicron infections,” Vespignani says.
That likely will hinge on what happens in other countries in the middle of this year. While the Northern Hemisphere experiences spring and summer weather that is less conducive to high rates of respiratory viruses like SARS-CoV-2, the Southern Hemisphere will be experiencing winter. Surges of coronavirus cases in those places could fuel the emergence of concerning variants that could spread around the world.
“Unfortunately this is something that might happen,” Vespignani says. But “the chances that the variant will be another nightmare are very, very slim.”
Virologists and epidemiologists like Vespignani study variants with particular attention to how transmissible they are, how readily they evade vaccine-induced immunity, and whether they cause more severe illness and death than previous versions.
While the omicron variant has been less severe than its predecessors, and vaccines have significantly reduced that severity further in people who have gotten their shots, the high transmissibility of the variant drove case rates to record highs in the United States.
Case counts and hospitalizations are on the decline, but death rates lag behind those metrics. More than 2,000 people are dying of COVID-19 a day in the U.S., according to the U.S. Centers for Disease Control and Prevention, although those numbers have begun to level off. By spring, Vespignani says the omicron wave probably will have brought around 100,000 deaths to the U.S. and about a million hospitalizations, due to the sheer volume of cases during this surge. The country last week reached a total of 900,000 COVID-19 deaths throughout the pandemic.
Source: Read Full Article
