Presently, many of Sweden’s 20,000 Parkinson’s patients are not receiving the treatment they need, and many of the most seriously ill receive incorrect or inappropriate therapy. With the new Manage PD tool and the PD Pal study, Per Odin, professor at Lund University and senior attending physician at Skåne University Hospital in Lund, hopes to be able to improve the care of Parkinson’s patients.
Every year, some 2,000 people in Sweden are diagnosed with Parkinson’s disease—a neurological movement disorder that means that nerve cells that produce dopamine slowly disappear, which leads to a dopamine deficiency in the brain. A person with Parkinson’s disease not only experiences problems with motor skills but also can suffer from a wide range of non-motor symptoms such as incontinence, constipation, pain, depression, apathy, anxiety, dementia and sleep disorders of various kinds.
“Over the past fifteen years, we have focused more on the non-motor symptoms, which are of course very important to pay attention to and treat if one wants to provide a decent quality of life. This especially applies to problems such as depression, anxiety, sleep problems, and daytime fatigue,” notes Per Odin, professor at Lund University´s strategic research area Multipark and senior attending physician at Skåne University Hospital.
Tablets are replaced with advanced therapy
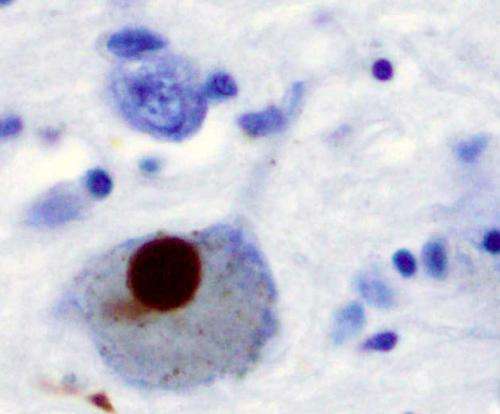
Presently today, there is no cure for Parkinson’s disease, only drugs that can improve the overall function and relieve discomfort. In the early stages of the disease, patients are often treated with tablets containing levodopa—a precursor amino acid that the body converts into dopamine. In step with the development of the disease, the tablets have an increasingly poor efficacy. The alternation between good condition and rigidity, between immobility and hypermobility, becomes increasingly difficult to deal with. The next step is to then switch to more advanced therapies such as pump treatment with the drug L-dopa or apomorphine, or deep electrode stimulation.
With deep brain stimulation, an electrode is surgically implanted into the targeted areas of the brain. The electrodes are connected to an implantable pulse generator, a type of pacemaker, that stimulates the brain electronically, and dampens stiffness and tremors.
With advanced therapy, most patients become significantly better and have a better quality of life. But not everyone who needs this has access to it:
“Today, about 1,100 patients in Sweden receive advanced therapies, which is a figure we estimate should be 2,000–3,000. Whether one receives treatment or not depends very much on where they live and which hospital they are receiving treatment from. There is a four times greater chance that a person will get advanced therapy if they live near the most diligent hospital compared to if one lives at the least diligent,” comments Per Odin.
Manage PD—an important tool for doctors
With the goal of ensuring that those who need access to advanced therapy will have such access, Per Odin and his colleagues have developed the Manage Parkinson’s Disease tool, Manage PD, which use in healthcare has now begun. The Manage PD tool can be most easily described as an automated algorithm. If the doctor is personally familiar with the patient, it takes about 3–4 minutes to enter various facts. The system suggests to the doctor what they should do: stop the current treatment, change the tablet treatment or alternatively refer the patient to a Parkinson’s treatment center, or if the patient is already in one, proceed further and explore if advanced therapy might be helpful for the patient.
“We sincerely hope that the Manage PD tool will become an aid to more patients receiving advanced therapy sufficiently soon enough, and thus improve their overall function and experience a better quality of life.”
The ultimate cost of using advanced therapies is zero
Per Odin believes that there are several reasons explaining why far too few Parkinson’s patients have access to advanced therapies. The treatments require more work and effort than simply continuing to give patients tablets, and it is difficult for the doctors to determine when it is really time for therapies. The financial costs are an influencing factor behind which decision is made. A pump treatment with L-dopa costs EUR 45,000 per year and deep electrode stimulation in the range of EUR 30,000 per operation.
In a collaboration with the Swedish Institute for Health Economics (IHE) in Lund, Per Odin’s research group recently published health economic data in an article that shows that the overall net cost of advanced therapies in Sweden is zero. With advanced therapy, patients can often stay longer at work and avoid hospitalization. The savings in providing medical care for patients are so great that they cover the full cost of the therapy.
“The difficulties are, of course, that the savings are primarily made in the municipalities financial accounts while the healthcare services incurs takes the costs. But just the knowledge that it is so I think can have a certain impact. We can give these patients and their relatives a better quality of life without a greater financial cost to the society when considered from an overall perspective.”
Specialist care comes home to the patient
Another important focus in Per Odin’s research is the patients who are in the final stage of the disease. They are often in such a bad situation that they are unable to walk without support and have difficulty getting themselves to a neurological department at a hospital. Many live in isolation, are treated incorrectly, and/or receive too little and sometimes even incorrect medication.
In a first European study, Per Odin and his colleagues found that these patients have a better quality of life if they have access to specialist care. A follow-up study named PD Pal is currently underway. Thirty patients in Sweden are participating; with 150 in the entire study overall.
“We send a Parkinson’s nurse to the patient’s home, who sees the patient on four occasions and together with the patient develops a treatment plan not only for the phase they are presently in but also for the future and even for the palliative final phase. They talk through how things will develop, what is most important for the patient, and how the treatment should best be structured.”
The palliative care offered can be improved
Region Skåne is participating in the study and funding it, which is expected to be completed in the spring and be evaluated next year.
“Many of these patients are not receiving adequate treatment. There is a whole lot that needs to be improved and we are also building in the palliative concept. It may sound sad, but it is positively meant—that in the final phase of the disease, the focus is no longer on maximum mobility but on the patient’s quality of life, which includes medication, provision of nutrition, where the patient should reside and additional related matters. The treatment of the non-motor symptoms becomes even more important in these stages,” stresses Per Odin.
Region Skåne has shown significant interest in the concept and sees it partly as a pilot project and then later a model for the university hospitals to reach out to patients to a greater degree than has occurred so far. A model that can also be used with other diseases and disorders with similar problems.
Source: Read Full Article
