Patients having intrauterine insemination for fertility treatment can be reassured that the use of cryopreserved sperm instead of fresh is not associated with inferior outcomes. The largest study of its kind, whose results are presented today at the 38th annual meeting of ESHRE, found no difference in pregnancy rates between cycles using cryopreserved or fresh sperm samples. The results of the study, presented today by Dr. Panagiotis Cherouveim from Massachusetts General Hospital and Harvard Medical School, U.S., were based on an analysis of 5335 intrauterine insemination cycles performed at his center between 2004 and 2021. “Patients undergoing IUI should be counseled about the non-inferiority of frozen sperm,” said Dr. Cherouveim.
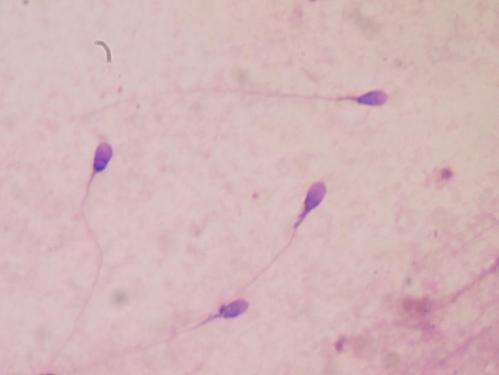
Cryopreservation has become the world’s favored method of sperm storage, and in most jurisdictions is a regulatory requirement for donor samples. This period of quarantine, which allows screening for infections before use, usually lasts up to six months (though for personal samples stored as a means of male fertility preservation may be longer). However, despite widespread use, there are concerns among patients that cryopreservation might reduce the viability of the frozen/thawed sperm cells, affecting their motility, structure and DNA content. “Contemporary data from intrauterine insemination cycles are still scarce,” said Dr. Cherouveim.
The study analyzed a range of outcomes following IUI treatments with either fresh or frozen sperm, which included a positive pregnancy test (hCG), clinical pregnancy, and miscarriage rate. The study also controlled for the type of ovarian stimulation either given or not given to women before their IUI treatment.
Results after adjustments for confounding variables found similar clinical pregnancy rates between those using fresh and frozen samples—although there were some minor differences noted in a sub-group of patients having pre-treatment ovarian stimulation with oral medications (clomiphene citrate or letrozole). However, when the analysis was limited to a first cycle of treatment, these differences were no longer evident. The only lasting difference was that time-to-pregnancy was slightly longer in the frozen sperm group than in the fresh. Thus, commenting on the results overall, Dr. Cherouveim said: “Although, specific subgroups might benefit from fresh sperm utilization and time-to-pregnancy might be shorter with fresh than frozen sperm, patients should be counseled about the non-inferiority of frozen sperm. No detrimental effect of sperm cryopreservation on IUI outcomes was noted.”
Commenting on the results, Dr. Cherouveim said: “The fact that our data did not reveal any significant difference in success between the utilization of fresh ejaculated and frozen sperm, except in a subgroup of patients given oral ovulation-inducing agents, is very reassuring to all involved.” He added that this might be especially welcome in single-mothers-by-choice and same sex couples for whom IUI with a cryopreserved sample might represent the one and only opportunity for conception in any given menstrual cycle. “This further highlights the importance of the sample’s quality,” he added.
Dr. Cherouveim added that the majority of cryopreserved sperm samples in this study came from an anonymous donor, which reflects the everyday practice of most fertility centers. Despite the necessity of sperm cryopreservation for certain regulatory and procedural processes—as well as the fact that donors are usually young, healthy and often fertile individuals with excellent semen parameters—patients often express concern over the duration of freezing or that the sample only represents a portion of the ejaculate. However, said Dr. Cherouveim, this study provides largely reassuring data on the non-inferiority of frozen sperm use.
Source: Read Full Article
