Mount Sinai researchers are the first in the country to use artificial intelligence (AI) combined with imaging, and clinical data to analyze patients with coronavirus disease (COVID-19). They have developed a unique algorithm that can rapidly detect COVID-19 based on how lung disease looks in computed tomography (CT scans) of the chest, in combination with patient information including symptoms, age, bloodwork, and possible contact with someone infected with the virus. This study, published in the May 19 issue of Nature Medicine, could help hospitals across the world quickly detect the virus, isolate patients, and prevent it from spreading during this pandemic.
“AI has huge potential for analyzing large amounts of data quickly, an attribute that can have a big impact in a situation such as a pandemic. At Mount Sinai, we recognized this early and were able to mobilize the expertise of our faculty and our international collaborations to work on implementing a novel AI model using CT data from coronavirus patients in Chinese medical centers. We were able to show that the AI model was as accurate as an experienced radiologist in diagnosing the disease, and even better in some cases where there was no clear sign of lung disease on CT,” says one of the lead authors, Zahi Fayad, Ph.D., Director of the BioMedical Engineering and Imaging Institute (BMEII) at the Icahn School of Medicine at Mount Sinai. “We’re now working on how to use this at home and share our findings with others—this toolkit can easily be deployed worldwide to other hospitals, either online or integrated into their own systems.”
This research expands on a previous Mount Sinai study that identified a characteristic pattern of disease in the lungs of COVID-19 patients and showed how it develops over the course of a week and a half.
The new study involved scans of more than 900 patients that Mount Sinai received from institutional collaborators at hospitals in China. The patients were admitted to 18 medical centers in 13 Chinese provinces between January 17 and March 3, 2020. The scans included 419 confirmed COVID-19-positive cases (most either had recently traveled to Wuhan, China, where the outbreak began, or had contact with an infected COVID-19 patient) and 486 COVID-19-negative scans. Researchers also had patients’ clinical information, including blood test results showing any abnormalities in white blood cell counts or lymphocyte counts as well as their age, sex, and symptoms (fever, cough, or cough with mucus). They focused on CT scans and blood tests since doctors in China use both of these to diagnose patients with COVID-19 if they come in with fever or have been in contact with an infected patient.
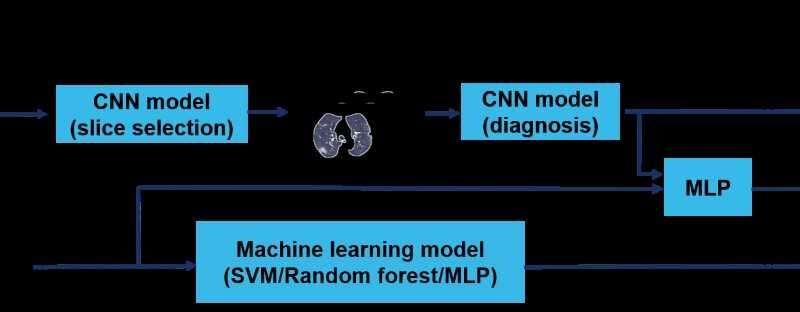
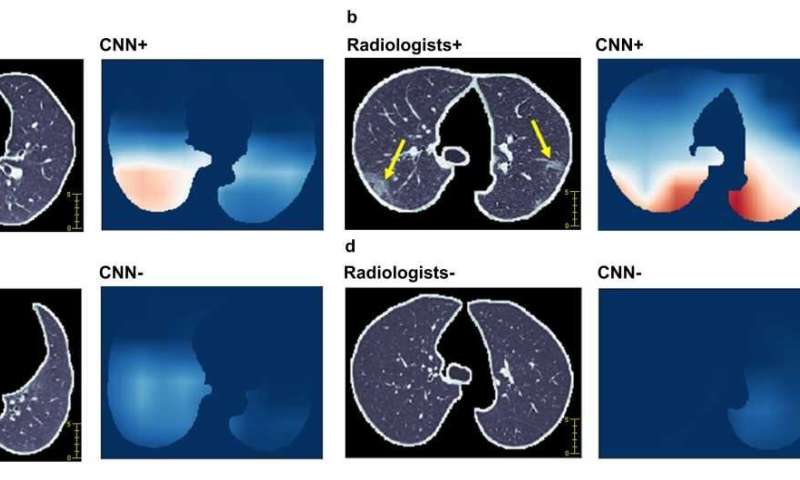
The Mount Sinai team integrated data from those CT scans with the clinical information to develop an AI algorithm. It mimics the workflow a physician uses to diagnose COVID-19 and gives a final prediction of positive or negative diagnosis. The AI model produces separate probabilities of being COVID-19-positive based on CT images, clinical data, and both combined. Researchers initially trained and fine-tuned the algorithm on data from 626 out of 905 patients, and then tested the algorithm on the remaining 279 patients in the study group (split between COVID-19-positive and negative cases) to judge the test’s sensitivity; higher sensitivity means better detection performance. The algorithm was shown to have statistically significantly higher sensitivity (84 percent) compared to 75 percent for radiologists evaluating the images and clinical data. The AI system also improved the detection of COVID-19-positive patients who had negative CT scans. Specifically, it recognized 68 percent of COVID-19-positive cases, whereas radiologists interpreted all of these cases as negative due to the negative CT appearance. Improved detection is particularly important to keep patients isolated if scans don’t show lung disease when patients first present symptoms (since the previous study showed that lung disease doesn’t always show up on CT in the first few days) and COVID-19 symptoms are often nonspecific, resembling a flu or common cold, so it can be difficult to diagnose.
CT scans are not widely used for diagnosis of COVID-19 in the United States; however, Dr. Fayad explains that imaging can still play an important role.
“Imaging can help give a rapid and accurate diagnosis—lab tests can take up to two days, and there is the possibility of false negatives—meaning imaging can help isolate patients immediately if needed, and manage hospital resources effectively. The high sensitivity of our AI model can provide a ‘second opinion’ to physicians in cases where CT is either negative (in the early course of infection) or shows nonspecific findings, which can be common. It’s something that should be considered on a wider scale, especially in the United States, where currently we have more spare capacity for CT scanning than in labs for genetic tests,” said Dr. Fayad, who is also a Professor of Diagnostic, Molecular and Interventional Radiology at the Icahn School of Medicine at Mount Sinai.
“This study is important because it shows that an artificial intelligence algorithm can be trained to help with early identification of COVID-19, and this can be used in the clinical setting to triage or prioritize the evaluation of sick patients early in their admission to the emergency room,” says Matthew Levin, MD, Director of the Mount Sinai Health System’s Clinical Data Science Team, and a member of the Mount Sinai COVID Informatics Center. “This is an early proof concept that we can apply to our own patient data to further develop algorithms that are more specific to our region and diverse populations.”
Source: Read Full Article
