More than 40% of hospitalized individuals with COVID-19 have diabetes. But why is having diabetes a major risk factor for a more serious COVID-19 illness? Researchers now are starting to put the puzzle together.
An international, multi-center observational study of more than 2,000 hospitalized COVID-19 patients found that certain attributes of diabetes, including high suPAR levels and high blood sugar levels, are correlated with worse COVID-19 outcomes.
The research, published in Diabetes Care, suggests that the patients with diabetes (approximately 33.5% of the study participants) have higher levels of inflammatory biomarkers compared to those without diabetes, exacerbating the effects COVID can have on the body.
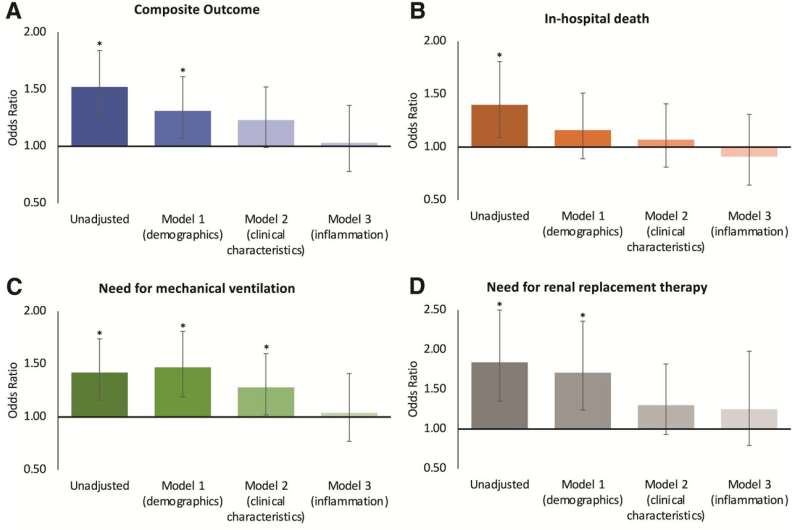
One inflammatory biomarker in particular, soluble urokinase plasminogen activator receptor or suPAR, is a circulating protein and notorious for its role in kidney failure and heart disease. This protein, in a multivariable analysis of other inflammatory markers, was the only one to show a significant impact on the relationship between diabetes and worse COVID outcomes.
COVID-19 outcomes of interest included in-hospital death, the need for mechanical ventilation and the need for renal replacement therapy.
The research team, led by Salim Hayek, M.D., a cardiologist at the University of Michigan Health Frankel Cardiovascular Center, Alexi Vasbinder, Ph.D., R.N., a post-doctoral fellow at the University of Michigan Health Department of Internal Medicine and Rodica Pop-Busui, M.D., Ph.D., an endocrinologist at University of Michigan Health and associate director for clinical research in the Elizabeth Weiser Caswell Diabetes Institute, also found that high blood sugar levels and higher insulin doses were independent predictors of worse COVID-19 outcomes.
“One main takeaway from this work is that the association between diabetes and COVID-19 outcomes is largely mediated by high inflammation in the body, as assessed by suPAR levels,” said Vasbinder.
According to the study, participants with diabetes had 20.7% higher suPAR levels than those without diabetes.
“However, the impact of hyperglycemia is independent of inflammation which means no matter what a patient’s suPAR levels indicate, having high blood sugar levels or high insulin doses will also result in more serious COVID-19 illness,” Busui added. This suggests that hyperglycemia affects COVID-19 outcomes through non-inflammatory processes, warranting further investigation.
These findings highlight the importance of a multidisciplinary approach to tackling the issue of diabetes and its relationship with worse COVID-19 outcomes, which is why Hayek and Busui work together to uncover high-risk factors and treat long COVID-19 as co-directors of Michigan Medicine’s adult COVID-19 Long Haul Clinic.
“To improve outcomes for this high-risk population, it’s critical to understand the relationship between diabetes, inflammation, and hyperglycemia in those hospitalized for COVID-19,” said Hayek.
However, understanding the interplay between these different variables, as well as their individual effects on COVID-19 outcomes, isn’t enough to improve the outlook for these patients.
Factors like age, body mass index and race need to be considered in order to provide the best quality, personalized care for at-risk patients, according to the study. Those with diabetes were older, more likely to be Black and have a high BMI.
“We found that these patients have nearly twice the comorbidity burden as it relates to hypertension, coronary artery disease, heart failure and chronic kidney disease, linking our early molecular studies of COVID and kidney now with outcomes ” said study author Matthias Kretzler, M.D., a nephrologist and leading kidney researcher at University of Michigan Health.
With all these factors at play, which ones seem to be the most important in identifying patients at highest risk for serious COVID-19 illness? For those with diabetes, suPAR levels, BMI, admission blood sugar levels, and age seem to be most significant, in that order. In fact, the study’s mediation analysis found that suPAR levels accounted for 84.2% of the effect of diabetes on worse COVID-19 outcomes.
“It’s important to note that given the small number of patients with type 1 diabetes in this study, the findings cannot be extended to them. For now, these results should be considered by providers treating patients with type 2 diabetes,” said Busui, who is also the recent president-elect of Medicine and Science as part of the 2022 American Diabetes Association Board of Directors.
Source: Read Full Article
