Redlining, a discriminatory mortgage lending practice instituted in the 1930s, resulted in health impacts that reverberate today, contributing to long-term environmental and asthma-related inequities that disproportionately affect Black Pittsburgh residents, according to a new analysis by University of Pittsburgh School of Public Health scientists.
The study, online now and scheduled for a coming print edition of the American Journal of Respiratory and Critical Care Medicine, is among the first to demonstrate that racism—rather than race—is an overarching socioenvironmental risk factor that appears to worsen asthma severity in Black people.
“We directly link racist loaning practices more than 80 years ago to the maintenance of poor environmental quality in the most redlined neighborhoods today,” said lead author Alexander Schuyler, an M.D.-Ph.D. student in Pitt’s Medical Scientist Training Program. “Our data, in turn, connects the higher pollution exposures to worsened asthma outcomes. In short, institutional racism—not race-based biology—is why many Black Pittsburghers experience severe asthma.”
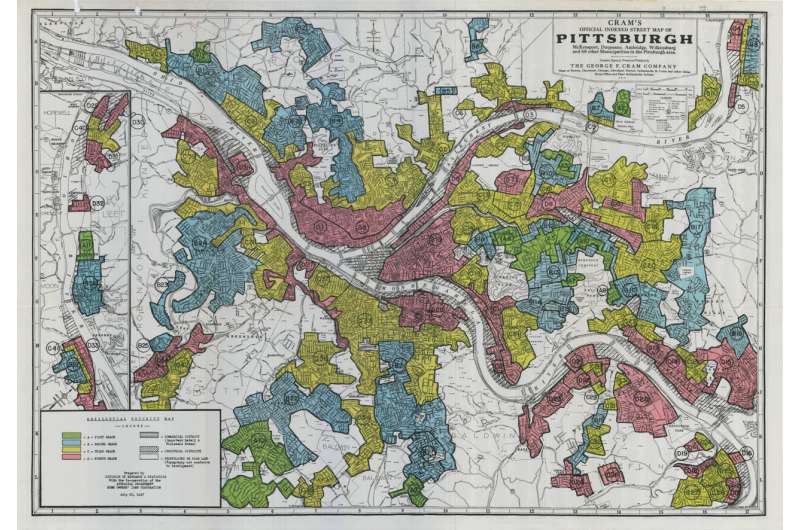
During the 1930s, the Home Owners’ Loan Corporation (HOLC) generated a four-tiered grading system for mortgage applications in more than 200 U.S. metropolitan areas, including Pittsburgh and Allegheny County. The corporation assigned an “A” score to neighborhoods it deemed “best” and a “D” score to neighborhoods it called “hazardous” for mortgage lending. “D” neighborhoods had the highest proportion of Black residents, resulting in Black loan applicants experiencing financial blacklisting—or redlining—for decades.
Schuyler partnered with Sally Wenzel, M.D., chair of Pitt Public Health’s Department of Environmental and Occupational Health and director of Pitt’s Asthma and Environmental Lung Health Institute at UPMC, to cross Allegheny County’s historically redlined neighborhoods with data from 1,034 participants in the Asthma Institute’s Asthma Registry. The registry, established in 2007, collects clinical and demographic information on patients with asthma.
By overlaying neighborhood-level data about different types of air pollution from multiple sources—industrial, vehicular, railroad and waterway—Schuyler and Wenzel determined that emissions of carbon monoxide, fine particulates, sulfur dioxide and volatile organic compounds all increased across HOLC grades, with “D” neighborhoods experiencing the highest pollution levels.
The worst asthma-related outcomes—including uncontrolled or severe asthma—followed the same trajectory and disproportionately affected Black asthma registry participants.
“Air pollution induces structural changes in the lungs, causes inflammation and damages cells lining the airway, all of which can exacerbate asthma,” said Wenzel. “So, seeing worse asthma in people living in neighborhoods with more pollution isn’t surprising. What struck me was the enduring legacy of redlining. We are still seeing the long-term effects of the loss of generational capital and neighborhoods labeled as ‘toxic.’ Institutional racism is something we, as clinicians, have to recognize as a real, continued threat to the health of our patients and one we must fight against.”
The researchers also found that registry participants living in “D” neighborhoods, especially Black participants, received lower-quality asthma-related health care. They were less likely to be prescribed stronger medications with worsening asthma or be referred for advanced care than their white “A” neighborhood counterparts.
Schuyler said this could reflect bias by health care providers, but could also arise from equations that factor in race when calculating pulmonary function, colloquially known as “race-norming.” This can result in a Black patient’s lung function being designated as normal, when had the patient been white, it would be considered poor enough to need additional medical attention.
Source: Read Full Article
