Every 30 seconds, a leg is amputated somewhere in the world due to diabetes. These patients often suffer from neuropathy, a loss of sensation in the lower extremities, and are therefore unable to detect damage resulting from an ill-fitting prosthesis, which leads to the amputation of a limb.
In Biomicrofluidics, Canadian scientists reveal their development of a new type of prosthetic using microfluidics-enabled soft robotics that promises to greatly reduce skin ulcerations and pain in patients who have had an amputation between the ankle and knee.
More than 80% of lower-limb amputations in the world are the result of diabetic foot ulcers, and the lower limb is known to swell at unpredictable times, resulting in volume changes of 10% or more.
Typically, the prosthesis used after amputation includes fabric and silicone liners that can be added or removed to improve fit. The amputee needs to manually change the liners, but neuropathy leading to poor sensation makes this difficult and can lead to more damage to the remaining limb.
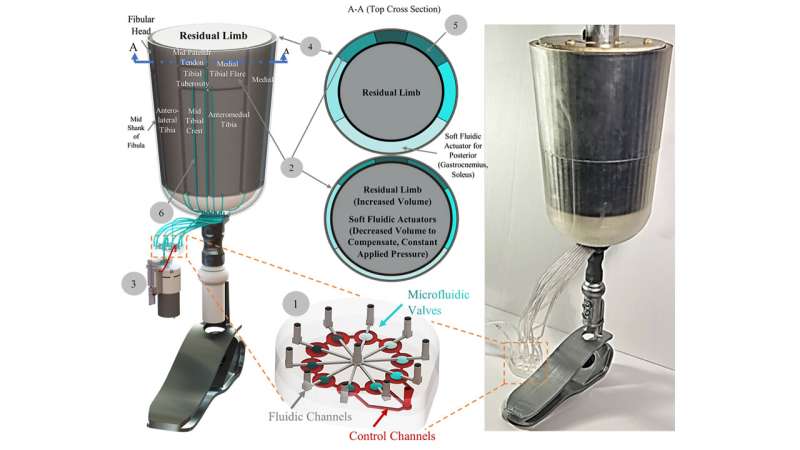
“Rather than creating a new type of prosthetic socket, the typical silicon/fabric limb liner is replaced with a single layer of liner with integrated soft fluidic actuators as an interfacing layer,” said author Carolyn Ren, from the University of Waterloo. “These actuators are designed to be inflated to varying pressures based on the anatomy of the residual limb to reduce pain and prevent pressure ulcerations.”
The scientists started with a recently developed device using pneumatic actuators to adjust the pressure of the prosthetic socket. This initial device was quite heavy, limiting its use in real-world situations.
To address this problem, the group developed a way to miniaturize the actuators. They designed a microfluidic chip with 10 integrated pneumatic valves to control each actuator. The full system is controlled by a miniature air pump and two solenoid valves that provide air to the microfluidic chip. The control box is small and light enough to be worn as part of the prosthesis.
Medical personnel with extensive experience in prosthetic devices were part of the team and provided a detailed map of desired pressures for the prosthetic socket. The group carried out extensive measurements of the contact pressure provided by each actuator and compared these to the desired pressure for a working prosthesis.
All 10 actuators were found to produce pressures in the desired range, suggesting the new device will work well in the field. Future research will test the approach on a more accurate biological model.
The group plans additional research to integrate pressure sensors directly into the prosthetic liner, perhaps using newly available knitted soft fabric that incorporates pressure sensing material.
Source: Read Full Article
