Annual MRI screenings starting at ages 30 to 35 may reduce breast-cancer mortality by more than 50% among women who carry certain genetic changes in three genes, according to a comparative modeling analysis to be published Feb. 17, 2022, in JAMA Oncology.
The predictions involve pathogenic variants in ATM, CHEK2 and PALB2 genes—which collectively are as prevalent as the much-reported BRCA1/2 gene mutations. Authors of the study, published in JAMA Oncology, contend that their findings support MRI screening in some of these women earlier than existing preventive-care guidelines propose.
“Screening guidelines have been difficult to develop for these women because there haven’t been clinical trials to inform when to start and how to screen,” said Dr. Kathryn Lowry, an assistant professor of radiology at the University of Washington School of Medicine. She was the paper’s lead author.
The work was a collaboration of the Cancer Intervention and Surveillance Modeling Network (CISNET), the Cancer Risk Estimates Related to Susceptibility (CARRIERS) consortium, and the Breast Cancer Surveillance Consortium.
Using established breast-cancer simulation models, the researchers input age-specific risk estimates provided by CARRIERS and recent published data for screening performance. The CARRIERS data involved more than 32,000 breast-cancer patients and a similar number of patients who had no cancer.
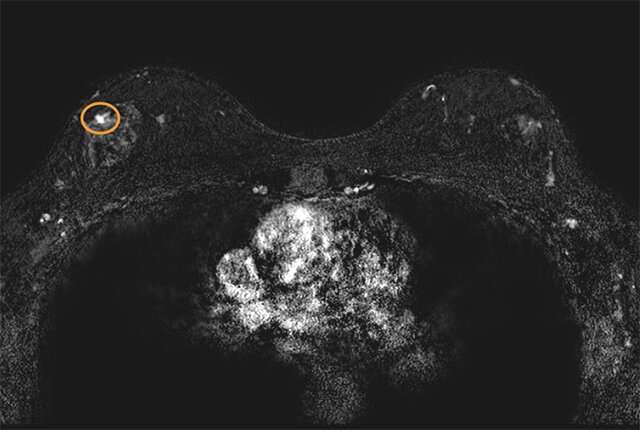
“For women with pathogenic variants in these genes, our modeling analysis predicted a lifetime risk of developing breast cancer at 21% to 40%, depending on the variant,” Lowry said. “We project that starting annual MRI screening at age 30 to 35, with annual mammography starting at age 40, will reduce cancer mortality for these populations of women by more than 50%.”
The simulations compared the combined performance of mammography and MRI against mammography alone, and projected that annual MRI conferred significant additional benefit to these populations.
“We also found that starting mammograms earlier than age 40 did not have a meaningful benefit but increased false-positive screens,” Lowry added.
Results from CISNET models have informed past guidelines, including the 2009 and 2016 U.S. Preventive Services Task Force recommendations for breast cancer screening in average-risk women.
“Modeling is a powerful tool to synthesize and extend clinical trial and national cohort data to estimate the benefits and harms of different cancer control strategies at population levels,” said Dr. Jeanne Mandelblatt, a professor at Georgetown Lombardi Comprehensive Cancer Center and a senior author on the paper.
The simulations in this study also predicted the volume of false-positive screening results and benign biopsies, per 1,000 women scanned, that would accompany the authors’ recommendations for annual MRIs starting earlier. Those projections translate to about four false-positive screening results and one to two benign biopsies per woman over a 40-year screening span, the authors said.
To realize a benefit of cancer screening guidelines based on genetic susceptibility, a woman would need to know she carries an implicated gene variant before receiving a disease diagnosis. More often it’s the case that a genetic test panel is administered after someone tests positive for cancer—too late to be of preventive value for the patient but potentially life-saving for blood relatives who could seek genetic testing.
“People understand very well the value of testing for variants in BRCA1 and BRCA2, the most common breast cancer predisposition genes. These results show that testing other genes, like ATM, CHEK2, and PALB2, can also lead to improved outcomes,” said Dr. Mark Robson. He is chief of Breast Medicine Service at the Memorial Sloan Kettering Cancer Center and a senior author on the paper.
The researchers hope their analysis will aid the National Comprehensive Cancer Network (NCCN), the American Cancer Society and other organizations that issue guidance for medical oncologists and radiologists.
Source: Read Full Article
