New data published today suggest that adding aerosolized hydrogen peroxide (aHP) to hospital infection prevention protocols can effectively reduce Clostridioides difficile infections (CDI), one of the most common healthcare-associated infections (HAIs), among patients in large, acute-care facilities. The findings, which offer the first, long-term evaluation of an aHP disinfection system for reducing CDI in a clinical setting, appear in the American Journal of Infection Control (AJIC), the journal of the Association for Professionals in Infection Control and Epidemiology (APIC).
“Our study showed that persistence in utilizing an aerosolized hydrogen peroxide system had a significant impact on reducing C. difficile infections hospital-wide,” said Christopher L. Truitt, Ph.D., Wayland Baptist University, and the paper’s lead author.
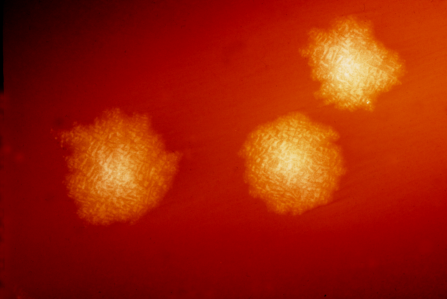
Individuals infected with C. difficile can be asymptomatic or have symptoms ranging from mild diarrhea to severe and life-threatening inflammation of the colon. According to the Centers for Disease Control and Prevention and The Joint Commission, C. difficile is responsible for 223,000 HAIs resulting in more than 12,000 deaths and $6.3 billion in costs in the United States annually. C. diff spores can be transmitted by environmental surfaces in hospital rooms, including bed handrails, equipment controls, and doorknobs, and are resistant to hand sanitizers and most disinfectants. Enhanced protocols for hand hygiene and environmental cleaning, along with improved antibiotic prescribing, are required to prevent C. diff spread and infection, but even with consistent implementation of these measures, the microbe is difficult to eradicate from hospital surfaces.
aHP disinfection systems offer a touchless, whole-room approach to enhance standard environmental cleaning protocols. Once placed in a room, the systems generate an aerosolized dry-mist fog that contains a specified percentage of hydrogen peroxide. The fog covers all exposed surfaces to kill any C. diff spores that remain after physical cleaning. To date, there is no long-term data evaluating the use of these systems.
Dr. Truitt and his colleagues retrospectively analyzed CDI rates at a large, acute-care facility in Philadelphia, Pennsylvania, over a 10-year period, to evaluate the effectiveness of an aHP disinfection system for reducing CDI. The researchers compared the incidence of healthcare-associated CDI (HA-CDI) at the facility prior to and following implementation of the system as an addition to standard CDI patient room-cleaning procedures following the discharge or transfer of patients with CDI.
Findings suggest that consistent use of an aHP disinfection system contributed to a significant and sustained reduction in HA-CDI rates. Over a 27-month period prior to implementation of the system, the facility recorded 120 HA-CDI. Following implementation, 72 cases were observed over a 33-month interval. This reflects a significant, 41% decrease in the facility’s HA-CDI rate—from 4.6 per 10,000 patient days to 2.7 per 10,000 patient days (p<0.001).
Over an additional five-year period during which the aHP system was consistently utilized along with an environmental cleaning program and other measures including antibiotic stewardship, researchers observed a 74% reduction in hospital-onset CDI.* Between January 2015 and December 2019, CDI rates consistently decreased from 5.4 per 10,000 patient days to 1.4 per 10,000 patient days.
Source: Read Full Article
