Medicine has two things to offer when viral pandemics hit: vaccines and therapeutics. While it is hard to undervalue the noble goal of rapidly developing and rolling out safe vaccines that effectively reduce disease severity, and potentially even rates of infection, some would argue that therapeutic options for COVID-19 have been underappreciated. While it is tough to find good estimates of how much funding has been made available for each strategy, it is probably fair to say that approving new drugs for COVID-19 has never been compared to the moon shot.
Needless to say, a few medical establishments have been taking a good hard look at which existing and inexpensive medicines already available might be effectively brought to bear against SARS. One such place is Nigeria, special in Lagos and Karu/Jos. The team of corresponding author Olufemi Emmanuel Babalola, from Bingham University’s Ophthalmology Department has recently published a paper to medRxiv in which they show that ivermectin has clear clinical benefit for COVID-19. Much like the controversial medicine hydroxychloroquine, ivermectin has been a battleground drug that is frequently in the news.
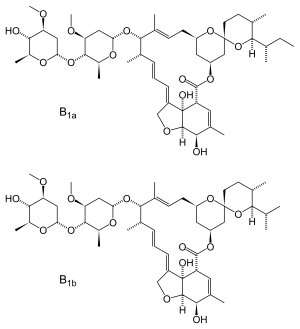
Ivermectin is quite extensively and safely used in many African nations for treating ocular onchocerciasis. Like so many important drugs, ivermectin has a broad spectrum of biological activity. It is antiparasitic, antibacterial and antiviral for several RNA viruses. In in-vitro studies, ivermectin gave a 5,000-fold reduction of SARS-CoV-2 in different kinds of cells, deduced from inhibition of RNA-dependent RNA polymerase, abolition of importin-α/β1 heterodimer nuclear transport of SARS-CoV-2 from the cytosol to the nucleus, or inhibition of viral mRNA protein translation.
The main problem with ivermectin has traditionally been that it wasn’t a good performer in silico. Kinetics simulations from cattle using a 10-fold higher dose than was used in vitro still failed to yield high enough simulated in vivo drug concentrations to achieve the IC50 (50% inhibitory concentration) value of 2.4uM that was required for in-vitro inhibition. On the other hand, later simulations with human pharmacokinetics in turn predicted 10-fold higher concentrations than the reported EC50 (50% effective concentration). Ivermectin is highly lipophilic, has a long half-life of around 85 hours, and a high volume distribution, indicating preferential lung and tissue accumulation. Pharmacodynamically, ivermectin is known to inhibit several important cytokines in a dose-dependent fashion.
Another important and timely review of the emerging efficacy of ivermectin was just published yesterday in Frontiers in Pharmacology. Among the authors of the paper is Paul Marik, who created the Front Line COVID-19 Critical Care Alliance (FLCCC) earlier this year to identify treatments for SARS-CoV-2. The paper describes successful treatments and prophylaxis for COVID-19 using ivermectin in “natural experiments” and trials in South America, Belize, Macedonia and Uttar Pradesh, among others. While many of these trials have been published in peer-reviewed journals, a majority are still on preprint servers, or in some cases, collections of anecdotes that haven’t even been written up.
While the text of the Frontiers article hasn’t yet been published, the abstract has been provisionally accepted and published. In fact, this is the way it is going to be now. Work will continue to be written up and offered to anyone who wants to try to extract whatever knowledge they can as soon as it is available, from whatever is reported—and who can argue with that?
One recent powerful anecdote is the case of a man who somewhat miraculously went into complete remission for Hodgkins lymphoma upon infection with SARS-CoV-2. While this case is undoubtedly an n of 1, similar cancer remissions after infections have been noted before in the literature. It has been suggested that one possible explanation, or at least useful theory, might be that the Hodgkins recovery could be related to antibodies generated against tumors as a side effect of SARS-CoV-2 infection. In fact, earlier this year, there was a study showing that after infection, a high prevalence of autoantibodies against immunomodulatory proteins including cytokines, chemokines, complement components and cell-surface proteins can be generated. While these autoantibodies were generally found to exacerbate disease severity in a mouse model of SARS-CoV-2 infection, in this man’s case, autoantibodies could have been his friend. Disclaimer: This is speculation.
Medicines may not be as glamorous as precision vaccines, but if they work, they are likely to be more robust against changes in the virus. In other words, they would be more resistant against point mutations, particularly against variants in the spike receptor binding domain (RBD) wherein vaccines painstakingly crafted to act against the unmutated genotype might no longer work as well, if at all.
By recreating variants in the lab for new viruses that are now spreading worldwide, binding activities can be readily determined and inhibitors quickly devised that block the spike-ACE2 interaction without blocking the natural ACE2 receptor activity we need to live. For example, in a recent study, Israeli researchers conducted in vitro evolution experiments to affinity maturate the RBD in the more contagious mutations S477N, E484K and N501Y now found in places like the U.K. and South Africa. In these experiments, binding affinity was already artificially enhanced by 600-fold, and in principle, should soon reach the maximum possible theoretical binding affinity and potentially the most highly infectious virus imaginable. While obviously scary stuff, at least in this case, we have a good understanding of who, exactly, is doing these studies, where they are doing them and why.
Source: Read Full Article
