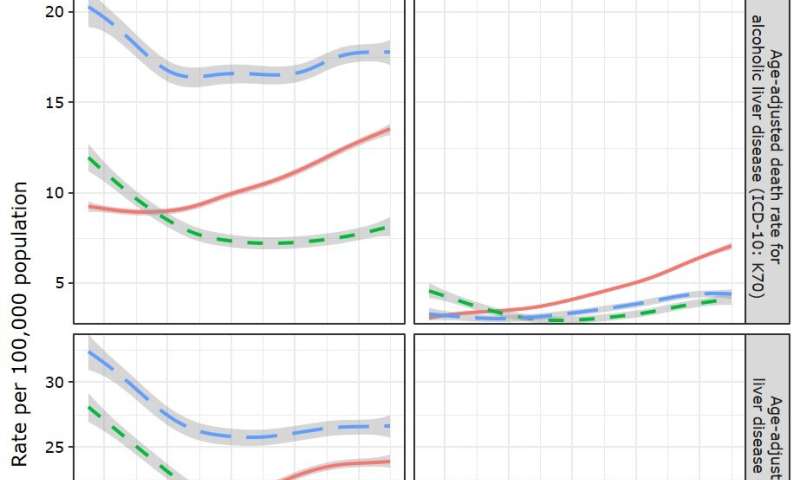
A new study in the American Journal of Preventive Medicine, published by Elsevier, identifies emerging patterns in the rate of and age at premature death from alcoholic (alcohol-associated) liver disease (ALD) in the United States over the last two decades. Significantly, the study documents that since the early 2000s, ALD death rates among non-Hispanic whites, particularly women, have increased more rapidly than rates among non-Hispanic blacks. Findings indicate that mortality is significantly impacted by socioeconomic and sociodemographic factors, the clinical course of ALD, and co-existing conditions.
“Empirical evidence from our study adds to the growing literature suggesting that previously large gaps between women and men in alcohol-related harms, including mortality, are narrowing,” explained co-investigator Aaron M. White, Ph.D., Senior Scientific Advisor to the Director, National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health, Bethesda, MD, U.S.. “Of particular concern is the largest increase that occurred among younger women ages 25—34. Because it usually takes 10 or more years of drinking to develop liver disease, premature mortality before 35 years of age is quite unusual and cause for serious public health concerns.”
Investigators drew death certificate data from the 1999—2018 Multiple Cause of Death database compiled by the National Center for Health Statistics. Each death certificate contains a single underlying cause of death, up to 20 additional contributing causes, and sociodemographic data. From 1999 to 2018, 281,243 individuals ages 25—69 died prematurely of ALD. Researchers looked at other factors reported as contributing to the cause of death: demographic characteristics (e.g., sex, race/Hispanic origin, marital status, education); the type of ALD (e.g., alcoholic fatty liver, alcoholic hepatitis; alcoholic cirrhosis of the liver); and comortalities (e.g., alcohol use disorder, tobacco use disorder, hepatitis C infection, diabetes, hypertension, injuries).
Highlights of the study’s findings include:
- Although men consistently had higher ALD death rates, gaps between men and women for ALD death rates have narrowed in the past two decades, especially among people ages 25—34 years. The rate ratio of men to women dropped from roughly 3:1 in 1999 to 2:1 in 2018.
- Women died of ALD on average about two to three years earlier than men, possibly due to the more rapid increase in alcohol misuse and relatively higher occurrence of alcoholic hepatitis in women at younger ages, coupled with higher prevalence of severe obesity among women.
- Years of potential life lost (YPLL), an indicator of premature death, increased more rapidly for women than men, especially after the economic recession in 2008. Since then, individuals with less than a college education, irrespective of sex, experienced a more rapid increase in ALD death rates than their college-educated counterparts.
- Compared to non-Hispanic whites, the age-adjusted ALD death rates among non-Hispanic blacks have been either declining or stagnant during this period or slowly increasing since 2008.
- Alcohol involvement in liver disease remained highest among Hispanics. Historically, sex disparities in drinking were more pronounced in Hispanics than in other racial/ethnic groups. The authors suggest that heightened rates among Hispanic women may be attributed to increases in female drinking driven by acculturation.
The authors conclude that the study supports population-level interventions and policies to reduce alcohol consumption and improve access to, and quality of, ALD treatment. Their findings may serve to raise public awareness of the rising levels of death from ALD and the groups at greatest risk, encouraging both physicians and patients to engage more frequently in discussions about alcohol consumption. To address narrowing sex gaps in premature death from ALD, greater emphasis should be placed on implementation of abstinence programs, early detection of ALD, and education about hazardous drinking levels for women.
Source: Read Full Article
