The coronavirus disease 2019 (COVID-19) pandemic has been endemic worldwide for over a year and has caused widespread disease resulting in millions of deaths. It finally appears as though it is beginning to be brought under control by a mixture of mass vaccination programs, repurposed drugs, and monoclonal antibody treatments. However, as the disease retreats, governments have begun to dismantle social distancing programs, restrictions on social gatherings, and other disease-preventing measures. Unfortunately, as variants of concern continue to emerge, including the increasingly worrying Delta strain of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), this may backfire.
In spite of the security vaccines offer, there is strong evidence that the SARS-CoV-2 Delta strain can not only still infect vaccinated individuals, but those individuals remain contagious. Rates of death fall significantly, but the disease is still a significant danger to over 80s and the immunocompromised.
Researchers from Utrecht University have been investigating the interactions between compliance social distance measurements, infection, and vaccination coverage in order to inform public health policy further. A research paper covering their work is available on the medRxiv* preprint server.
Variants
The waves of variants that spread over the globe, including the Alpha, Beta and Gamma variants, caused new restrictions to be introduced across Europe. Despite this, the Delta variant emerged in 2020 and quickly became the dominant strain, underscoring the danger and continued transmission despite the restrictions.
Vaccination
Vaccination programs showed success in countries like the United Kingdom and Germany but faced trouble in many others. Vaccine hesitancy is often mentioned in relation to the US, but other countries show far lower vaccine acceptance rates. Kuwait, for example, rests at 23.6%. In addition, more remote countries can suffer from logistical challenges, especially considering the need for constant refrigeration.
Modeling
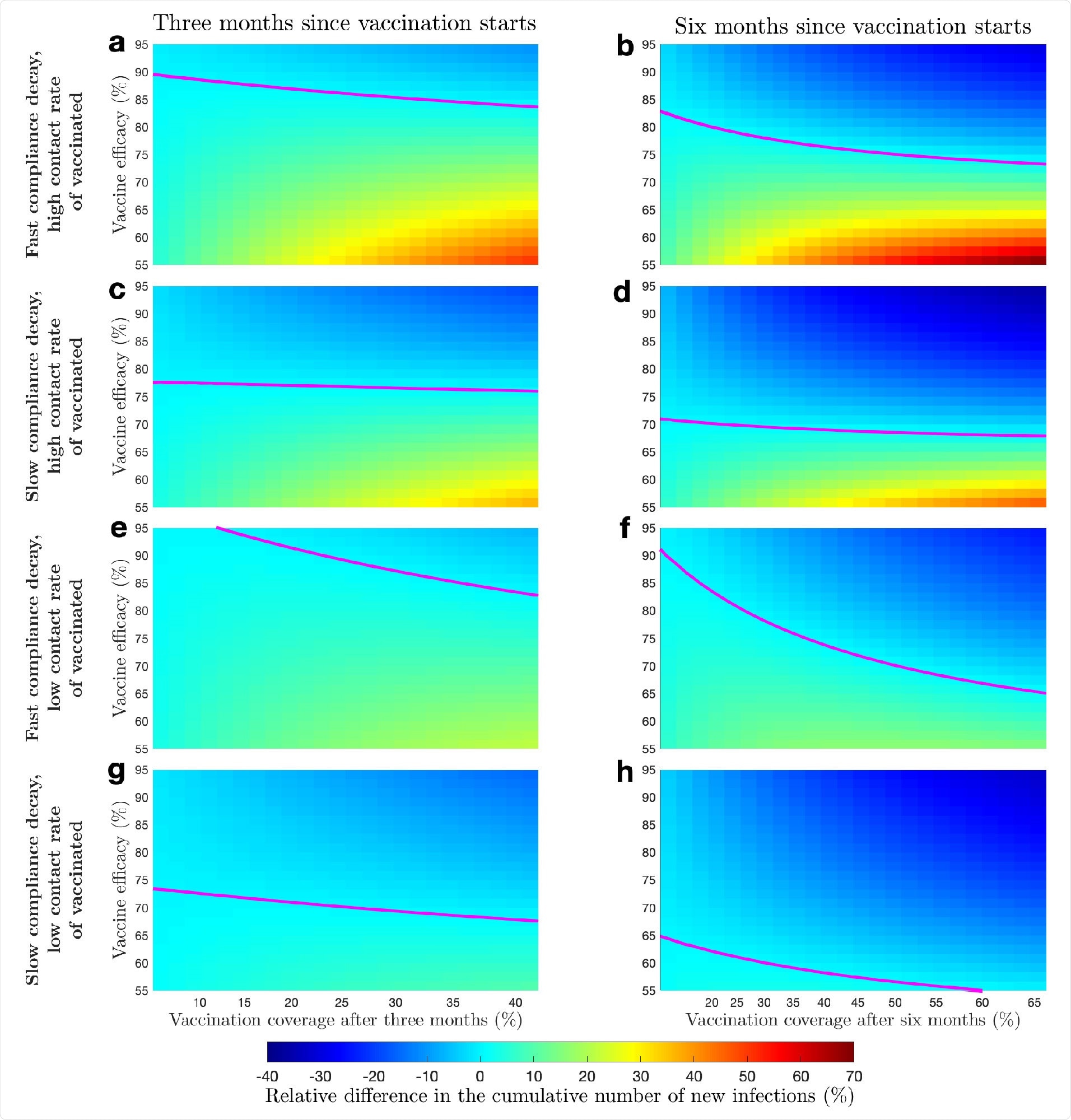
In order to examine the effect of the various factors, the researchers created a socio-epidemiological model of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission. They use a susceptible-exposed-infectious-recovered (SEIR) framework to model transmission.
This assumes the vaccine provides perfect protection to a fraction of individuals in the susceptible category and has no effect on any others. This is not an ideal model of reality – multiple studies have shown an intricate and complex relationship between infection, recovery, and the vaccine.
Rather than perfect protection, it is far more common for the vaccine to reduce severity and transmission likelihood. However, there are many other factors involved in the transmission, so some simplification is required.
The model is based upon a society currently undergoing a lockdown with limited contact between people and recommendations to reduce daily contact further. Non-vaccinated individuals are split into compliant and non-compliant to the lockdown, with the number of daily contacts based on these categories. Individuals will switch between the categories. Vaccinated individuals will not comply with social distancing measures. As cases of SARS-CoV-2 infection grow, more individuals will comply.
The transmission rate was based on the transmission of the original variant, Alpha, and Delta variant. To begin the modeling, the state of the epidemic and compliance was based on the Netherlands in November 2020 (prior to vaccination). The proportion of individuals in each category of the SEIR framework was decided by seroprevalence data, which set the recovered population at 8%. 65% of the population was set as compliant.
Vaccination rate
The authors set two vaccination rates based on different dates of sampling in the Netherlands. When the vaccination rate was set as fast, the population gained immunity quickly. On the other hand, when the vaccination rate was set as slow, they still gained immunity, just slowly.
The researchers found that when compliance with social distancing and other measures reduces as vaccine coverage grows, the new rate of transmission is strongly dependant upon the speed of the vaccine rollout. Slow vaccine rollout combined with low compliance actually shows worse short-term transmission than no vaccination at all, and could even result in another 'wave' or peak of instances of COVID-19.
The authors' findings are supported by previous studies suggesting similar effects of waning compliance. The authors highlight the importance of their findings in informing public health policy and urge social distancing measures and other restrictions to be maintained during the early phases of vaccination programs.
For many countries, this advice may come too late, but it could be invaluable advice for those that remain.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behaviour, or treated as established information.
- Teslya, A. et al., (2021) The importance of sustained compliance with physical distancing during COVID-19 vaccination rollout, medRxiv, preprint server. https://doi.org/10.1101/2021.09.22.21263944, https://www.medrxiv.org/content/10.1101/2021.09.22.21263944v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibody, Coronavirus, Coronavirus Disease COVID-19, Drugs, immunity, Monoclonal Antibody, Pandemic, Public Health, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Vaccine, Virus

Written by
Sam Hancock
Sam completed his MSci in Genetics at the University of Nottingham in 2019, fuelled initially by an interest in genetic ageing. As part of his degree, he also investigated the role of rnh genes in originless replication in archaea.
Source: Read Full Article
