Oxygen therapy can save the lives of children with pneumonia, but careful monitoring is needed to reduce harm, avoid over-reliance and protect supply.
These are among some of the key findings to emerge from a four-year-long study of children hospitalized with severe pneumonia in East Africa.
Led by researchers at Imperial College London, the Children’s Oxygen Administration Strategies Trial (COAST) set out to look at the evidence base for oxygen therapy. The team assessed whether liberal use of oxygen therapy had a measurable impact on child deaths, as well as comparing the impact of different forms of oxygen delivery on mortality.
The researchers say their findings highlight that a blanket approach of providing immediate oxygen therapy may not be appropriate for all patient groups, and that an over-reliance on oxygen can drain limited supplies unnecessarily in hospitals with low resources.
“There’s a big gap between what’s recommended and what’s happening in practice,” explained Professor Kathryn Maitland, Professor of Tropical Pediatric Infectious Disease at Imperial and head of COAST.
“There are still a lot of issues over who needs oxygen, how much to give and when to start and stop. Ultimately, oxygen is expensive, it can be difficult to deliver to patients and to monitor properly, and in high concentrations it can even be toxic to cells—so it’s important that there is an evidence base for its use.
“We hope that this research stimulates further debate and exploration of how we can best care for children with severe pneumonia, particularly in low resource settings.”
Leading cause of mortality
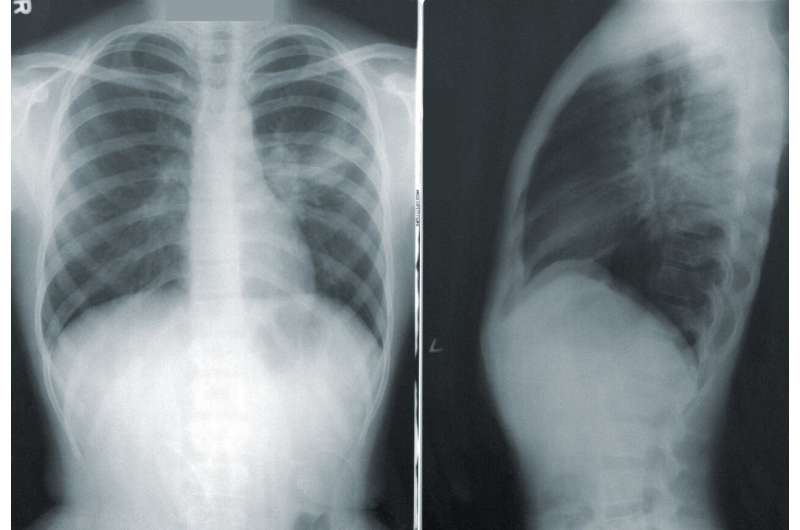
Along with diarrhoeal disease, pneumonia is one of the leading causes of mortality for children under the age of five, globally—with a high mortality rate for children admitted to hospital.
Reduced oxygen supply to the body, termed hypoxaemia, is a life-threatening complication of pneumonia and oxygen therapy is recommended for hospitalized children with low levels ofNO2 in the blood (typically below 92%). While simple monitors like a pulse oximeter can provide reliable measurements ofNO2 levels, they may often be unavailable in rural areas, leading to visible clinical signs being used as an unreliable proxy for lowNO2. In hospital settings this can result in children receiving oxygen when it may provide limited therapeutic benefit.
“Oxygen is recommended to children with pneumonia, and ideally, if you measure theNO2 saturation and it is low, you should be giving these children oxygen,” explained Professor Maitland.
“But a lot of hospitals do not have adequate monitors so they allocate oxygen based on clinical signs, which are a poor indicator. So you could be giving a very large number of hospitalized children oxygen, and they may be gaining very little, or even no benefit from it.”
The COAST study
As part of the study an international team of researchers and clinicians, led by Professor Maitland, recruited more than 1,800 children hospitalized with severe pneumonia in Kenya and Uganda—roughly half of which had severe hypoxaemia.
All children with severe hypoxaemia (n=388), withNO2 levels below 80%, were randomised to receive standard ‘low flow’ oxygen therapy (LFO) via a mask connected to an oxygen cannister, or to receive high flow nasal therapy (HFNT), via a breathing tube to the nose delivered by a specialist respirator.
For those with moderate hypoxaemia, roughly half of the children (n=727) did not immediately receive oxygen but were carefully monitored—the ‘permissive hypoxaemia’ group. If at any time theirNO2 levels dropped below a threshold of 80% they were immediately started on oxygen therapy. The remaining children were randomised to receive either LFO or HFNT, as a comparison.
After 48 hours, the team found that the majority of children, across all groups with moderate hypoxaemia no longer required oxygen and only 15% of the permissive hypoxaemia group ever needed oxygen. Despite this, there was little difference in mortality rates irrespective of whether they initially receivedNO2 therapy immediately or not: 1.1% for HFNT; 2.5% for LFO; and 1.4% for permissive hypoxaemia.
In addition, they found that among children receiving oxygen therapy, those receiving HFNT had a 40% lower mortality rate after 48-hours compared to standard LFO, across all groups. The researchers say that these findings were not conclusive, but they should stimulate further exploration of non-invasive respiratory support for children with severe pneumonia in hospitals where there is no access to ventilators (invasive mechanical respiratory support).
Following a recommendation by the independent Trial Steering Committee that it was not feasible for the trial to continue to its conclusion—due to multiple disruptions which caused the study to stop and restart—the trial ended in February 2020.*
The researchers stress that while the trial was ended early, it shows that a ‘watch and wait’ approach of active monitoring may be most appropriate for patients for whom oxygen may provide limited benefit, preserving limited supplies for those patients who can benefit most. They highlight that further research is needed to clarify patient care pathways in hospital settings with limited resource.
“In those with a moderate reduction in oxygen levels, we found that there was no detrimental effect from not immediately receiving oxygen,” explained Professor Maitland.
“While the trial ended early, we can say that the concerns raised over delaying oxygen therapy for children at lower risk in the trial were not realized. This study challenges the current thinking that oxygen is held as absolutely critical in keeping people alive.
“What we’ve shown in this trial is that, under certain circumstances, not providing oxygen immediately likely did not increase mortality, and that further research should be carried out on the best way to manage care in resource limited settings.
“We have also shown it is possible to provide assisted respiratory support with HFNL on the pediatric wards in Africa with a strong possibility that this may reduce deaths from severe pneumonia.”
The Children’s Oxygen Administration Strategy Trial (COAST) began in February 2017. It was designed to help children with pneumonia to receive the best possible treatment and have the best chance of survival. Pneumonia is one of the main causes of death in young children in Africa.
Following a recommendation by the independent Trial Steering Committee that it was not feasible for the trial to continue to its conclusion, the trial ended in February 2020.
The trial had been halted and restarted several times in Uganda as a result of a campaign that called the trial’s safety into question, and this disruption ultimately made it difficult for the trial team to carry on with their work.
The trial was regularly reviewed by an independent Data and Safety Monitoring Board, which conducted four detailed reviews, each finding there were no safety concerns and recommending that the trial should continue.
The mortality rate for children enrolled in the trial, as analyzed by the Data and Safety Monitoring Board, was significantly lower than would be expected for children receiving hospital treatment for pneumonia in Africa.
Source: Read Full Article
