It’s been six months since the UK entered lockdown.
And with life slowly opening back up, at least for now, the events of March can sometimes seem distant and otherworldly. But the effects of the COVID-19 pandemic, and the devastating impact it’s had on cancer services, remain.
We’ve covered some of COVID-19’s consequences before. But for the first few months all we had were snapshots and relative estimates. Six months on, we’ve got a much clearer picture how cancer services were affected, and how well they’re recovering.
Here’s what we know.
Screening
Let’s start with screening, which was badly affected by the COVID-19 pandemic, with bowel, breast and cervical screening programs all put on hold at the beginning of lockdown.
And with around 210,000 people being screened each week in the UK before the pandemic, the backlog of people waiting for screening has stacked up quickly—we put the figure at around 3 million so far.
The good news is that some programs have now restarted in some way. But given the number of people needing to be screened, it may be some time before they are back on track. And as health is a responsibility for each Government across the UK, timelines for restarting will be slightly different in each UK nation.
Getting screening up and running and addressing the backlog poses significant and unique challenges for each program. For cervical screening, services are prioritizing people who had an abnormal screening result before lockdown, followed by people who had an abnormal result the year before and then those who didn’t receive a screening invite during the pandemic.
While breast screening is restarting, capacity is lower due to infection control requirements and the additional cleaning that needs to take place. There’s also work to be done to ensure that mobile breast screening units, which are particularly important in more remote areas of the UK, can deliver breast screening safely.
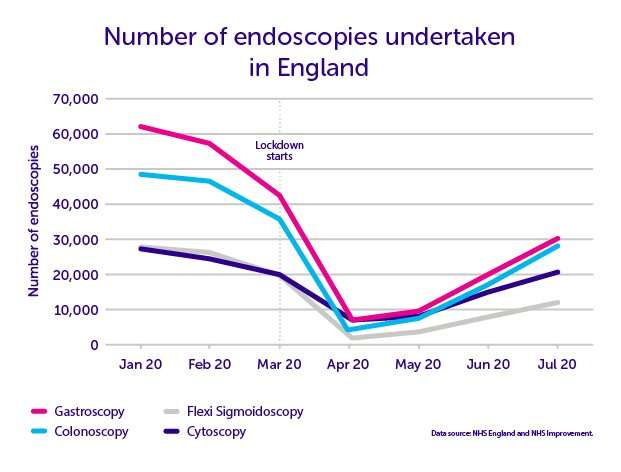
Finally, bowel screening. The main area of concern for this program is not the screening test itself, because it’s a test people do at home, but the follow-up test: colonoscopy. Colonoscopy is a type of endoscopy, which uses a camera to look inside the body.
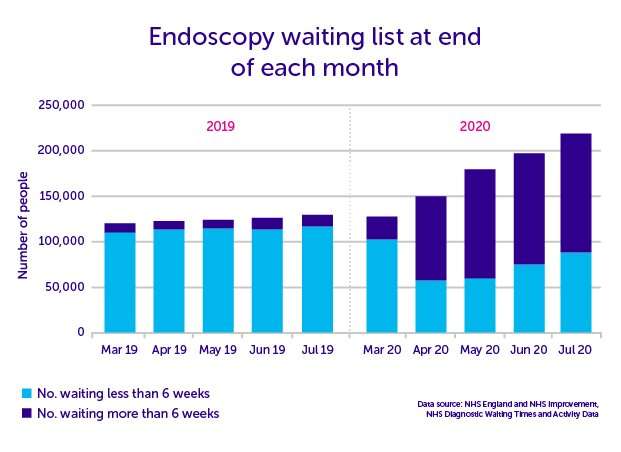
With endoscopy services among the worst hit, clearing the backlog of people waiting for a bowel screening follow up test is not easy. And it’s been made more challenging as the backlog of those referred by their GP for an endoscopy grows too.
But while it’s vital to get invites out, getting screening back on track will depend on people taking up their invite. We’ll be monitoring uptake closely over the next few months, as well as looking to see if the pandemic has changed who takes part in screening.
Cancer diagnosis
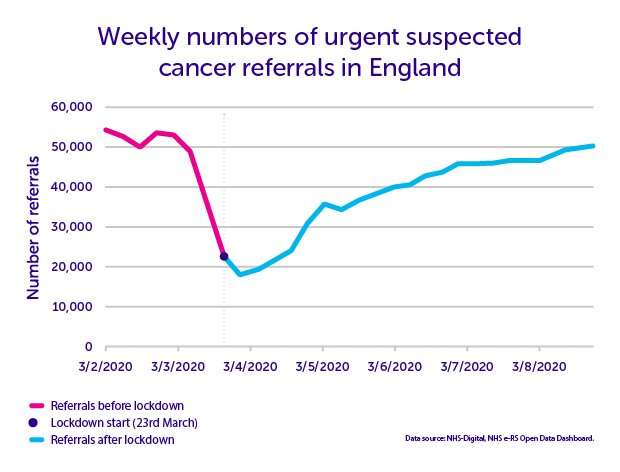
Another area that was heavily affected by COVID-19 was the number of people being urgently referred with suspected cancer symptoms. Between April and August, we’ve estimated that around 350,000 fewer people were referred than normal in the UK.
This drop is largely because fewer people went to their GP with symptoms that might be cancer, but we also know that some GPs were reluctant to risk sending people to hospitals during the height of the pandemic. The good news is the figures are steadily improving, but they’re still slightly lower than before lockdown.
But with 350,000 fewer people being referred since lockdown began, getting back to ‘normal’ isn’t enough. We need to see the number of referrals rise above pre-COVID figures to address the backlog of people who didn’t go to their GP or weren’t referred during lockdown and who still have concerns or symptoms.
Urgent suspected cancer referrals are only one part of the picture, with normally around a third of people with cancer being diagnosed through this route. But they’re a good indication of how many people are coming forward with symptoms and cancer services are doing across the UK , alongside other figures.
Because for cancer services to fully recover, we also need the people being referred to get the tests they need in a timely manner.
Which brings us to diagnostic tests. Most of the figures we have cover all diagnostic test activity and aren’t specific to cancer. But we can see that the number of tests that are often used to diagnose cancer—endoscopies (colonoscopy, flexi-sigmoidoscopy, cystoscopy and gastroscopy), CT scans, ultrasound and MRI—all dropped at the start of lockdown.
In England, there was a 39% drop in the number of these seven key diagnostic tests between March and July this year, which is equivalent to around 3.2 million fewer tests compared to the same period last year. The figures have started to recover since they hit their lowest point April, as you can see from the endoscopy figures below, but we’re still not back to last year’s activity.
And this drop in activity, combined with the additional safety measures put in place during the pandemic, has had a knock on effect on how long people are waiting for tests.
In England, the number of patients waiting six weeks or more for a diagnostic test has risen significantly since April, with the biggest increase in May . And while the number of patients waiting six or more weeks has fallen slightly in July, there are still 12 times more patients waiting six weeks or more for one of the seven key diagnostic tests compared to the same time last year.
Data released for Scotland and Northern Ireland shows a similar picture.
Cancer treatment
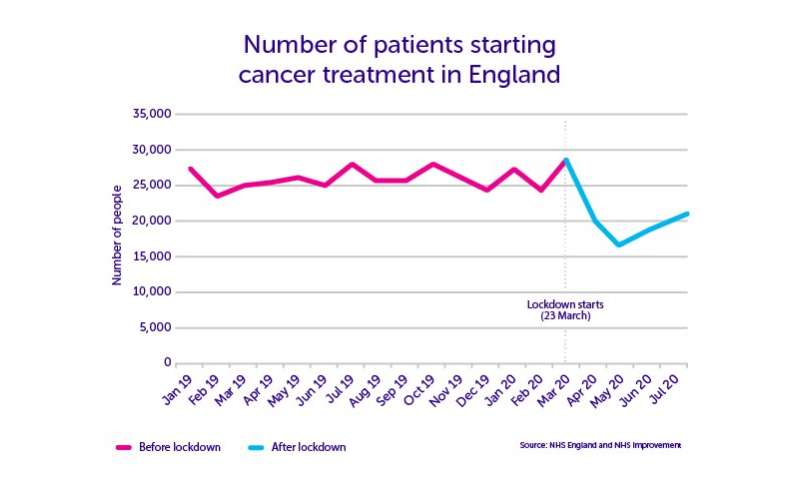
We’ve got less data when it comes to the impact of COVID-19 on cancer treatment. But since lockdown we know there’s been a decrease in the number of people beginning treatment since April 2020, with a 37% drop in the number of patients beginning treatment in England in May compared with the same period last year.
The spike in March corresponds to the period just before lockdown in England, when clinicians were trying to get as many people as possible through treatment before the pandemic really hit. Sometimes these March figures are grouped together with April and May and quoted as a lockdown figure.
For example, one figure used in the media is that over 65,000 people started cancer treatment from March to May—85% of the number that started in the same period last year. But this can be slightly misleading, as the spike in March masks the subsequent drop.
And the real impact of COVID-19 on cancer treatment overall may be masked by the fact that some people, including those who started treatment before the pandemic, have had changes to their treatment—radiotherapy before or instead of surgery for example. This has been done for good reasons, but the long-term impact on patient outcomes is hard to predict, especially since we don’t yet have good data on how many people have had their treatment switched in this way.
In a survey we conducted in May, one in three cancer patients said their treatment had been impacted by the effects of COVID-19 on the health system. And four in 10 people said their tests—including those to find out whether their cancer has spread or returned—had been affected.
These delays had a big impact on people’s mental health, with around seven in 10 people who experienced delays feeling more frustrated and anxious.
The good news is there are definite signs that cancer treatment is beginning to recover, with the number of patients beginning treatment rising in June and July, although it’s still around 24% lower than the same time last year.
Looking to the next few months, one challenge for the NHS will be ensuring it has enough capacity to treat the backlog of patients who receive their diagnosis as diagnostic services recover.
Building better cancer services
The last six months has been one of the most challenging period in the history of the NHS. And thanks to the dedication of healthcare staff and the work of cancer recovery planners in all four UK nations, the figures are moving in the right direction.
But there’s a lot of work that still needs to be done to get cancer services back on track and to ensure that cancer screening, diagnosis and treatment will not be as severely impacted by any future waves of COVID-19.
We’ve written before about what needs to happen to make sure that everyone gets the care they need, when they need it. But it’s not just about getting back on track, we need to aim higher. Cancer services weren’t functioning perfectly before the pandemic, with survival for many cancer types lagging behind comparable countries.
Now is the time to not only rebuild our cancer services, but to make them world-class. To make sure that everyone with cancer gets the diagnosis, treatment and care they deserve. And central to this transformation is a strong cancer workforce.
Source: Read Full Article
