The COVID vaccine rollout is now underway in Australia and around the world. It’s incredible we’ve been able to develop and produce safe and effective vaccines so quickly—but the current crop of vaccines might not protect us forever.
Fortunately, researchers are already developing and testing booster shots. So what are booster shots, and when might we need them?
First a prime, then a boost
The first time you give someone a dose of vaccine against a particular infection, it’s called a prime. You’re getting your immune response ready to roll.
Each time you give another dose against that same infection, it’s called a boost. You’re building on immunity you already have from the first dose.
Importantly, giving smaller doses in multiple shots is often better than a large dose of vaccine in a single shot. This is because our immune system builds on our immunity like bricks in a wall; each level needs to be laid before the next layer is built.
Booster shots take advantage of a phenomenon called “immunological memory”. Our immune cells essentially remember vaccines we’ve previously received, and respond much more quickly and vigorously to subsequent shots, building our immunity to levels at which we can be confident we’ll be protected.
When might I need a boost?
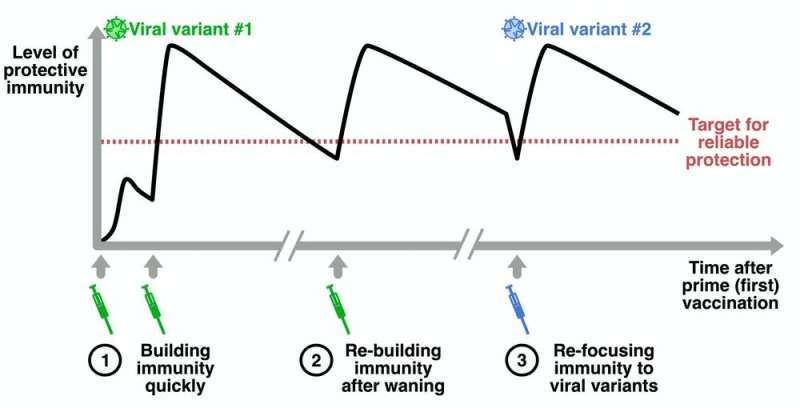
There are three different situations in which you might need a boost.
First, several doses of a vaccine can be given relatively quickly, one after another, to rapidly build someone’s immunity against a given infection. A good example is the whooping cough vaccine. It’s initially given at around two, four and six months of age to rapidly build immunity in infants, who are most at risk from whooping cough.
This is also the approach most COVID vaccines use. The first shot gets your immune system going but immunity is unreliable. The second shot leads to more consistent protection.
Second, we can give a booster shot if immunity drops over time, or “wanes,” to restore someone’s immunity to optimal levels. For example, we know immunity to tetanus can drop over time, so we recommend tetanus boosters every ten years.
Immunity appears to be strong three months after the Moderna vaccine and six months after the AstraZeneca vaccine, but we don’t yet have a full picture of how long immunity to COVID-19 lasts after vaccination. Scientists will continue to monitor this to determine if and when we’ll need these type of boosters for COVID.
Third, if the virus “mutates” or changes substantially over time, this can make it challenging for our immune cells to recognize the virus, effectively lowering our immunity again. A good example here is the influenza vaccine. The ‘flu virus can change a lot from year to year so, to make sure immunity remains high, we give annual boosters tailored to new strains.
On the front foot with viral variants
SARS-CoV-2, the virus that causes COVID-19, has already undergone a number of changes. We’re still learning how this might affect the efficacy of different vaccines.
But vaccine manufacturers are already adjusting their COVID vaccines to better target new variants. Moderna, for example, has just administered the first doses of an updated vaccine to volunteers in a new clinical trial. They’re intending to find out how well it works against B.1.351, the variant first identified in South Africa.
The updated vaccines tweak the “antigen”—the molecule used by our immune cells to target a specific virus. But they can use the same basic design and manufacturing processes.
As a result, they probably won’t have to go through the full gamut of clinical testing again. Regulatory hurdles are similarly streamlined with updated ‘flu vaccines.
Rapid development of these updated vaccines will put us on the front foot in our fight against COVID-19.
More of the same, or something a little different?
With boosting, you can end up with a higher level of immunity if you wait longer between doses. This is because our immune cells need a rest before they can respond to additional doses. We’ve seen this with the AstraZeneca vaccine where a longer delay between doses, up to 12 weeks, leads to much better protection.
It’s also possible we could generate greater immunity if we use different vaccines, one after the other, rather than repeating the same vaccine. This is called heterologous prime boosting.
We’re not sure why a mix-and-match approach can be more potent. But it’s possible combining two different vaccines—which give the same antigen target but stimulate the immune system in different ways—could better focus our immune cells’ attention on the right target.
We haven’t really taken advantage of heterologous vaccines in real-world settings yet. The first clinical heterologous vaccine was an Ebola vaccine approved in May 2020, while the Sputnik V COVID vaccine is also a heterologous vaccine.
But that could change. While there are now multiple approved COVID vaccines, vaccine rollout has been challenging. In the United Kingdom, the official policy is to use the same vaccine for both shots. But if the vaccine used for the first shot is not known or not available, people can still receive a booster with what is available.
Meanwhile, a clinical trial in the UK is evaluating the immune response when the Pfizer vaccine is followed by the AstraZeneca vaccine, and vice versa, as compared two doses of the same vaccine.
Source: Read Full Article
