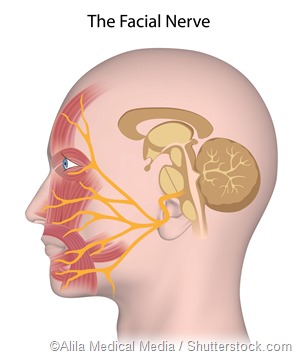
 Paralysis of the facial nerve may arise due to infection, inflammation, surgery, trauma and tumors. Damage to this nerve, which is the seventh cranial nerve, may be uni- or bilateral. It results in facial muscle weakness and/or drooping of the face.
Paralysis of the facial nerve may arise due to infection, inflammation, surgery, trauma and tumors. Damage to this nerve, which is the seventh cranial nerve, may be uni- or bilateral. It results in facial muscle weakness and/or drooping of the face.
This is a very unfavorable condition to have, whether temporary or permanent, because the face and its expressions play pivotal roles in the revelation of personality and character. For example, smiling, which is usually an amicable expression, may be twisted with facial nerve paralysis and inadvertently portray a cynical expression to someone unaware of the patient’s condition.
Managing facial nerve paralysis is fairly complex, and may involve pharmacotherapy in addition to surgery, with the help of static and dynamic techniques to reanimate the face, and physiotherapy for retraining the neuromuscular functioning of the face. Decompression is required when the facial nerve is compressed anywhere along its path through the skull. Decompressing the facial nerve may be done through one of three approaches or a combination, where applicable. These include the transmastoid, middle fossa and translabyrinthine approaches.
Transmastoid facial nerve decompression
If the damage to the facial nerve is localized near the mastoid or tympanic segments of the nerve, then the transmastoid approach may be used. The decompression is done over 180 degrees of the nerve’s circumference. Critical surgical landmarks for this procedure are the digastric ridge (i.e. a ridge of bone, which is posterior to the facial nerve and medial to the tip of the mastoid), the fossa incudis and the lateral semicircular canal. During the process, the incus may be replaced by an interposition graft. This allows for more extensive decompression of the nerve.
Middle fossa and translabyrinthine facial nerve decompression
Facial nerve injury extending to the labyrinthine segment of the nerve may require decompression via the middle fossa approach. In this approach, the semicircular canal, greater superficial petrosal nerve and the vertical crest that separates the superior vestibular and facial nerves from each other, are all used as crucial surgical landmarks.
Middle fossa facial nerve decompression may be done alone or it may sometimes be combined with the transmastoid procedure. This combination is especially utilized for facial nerve compression that arises due to trauma to the temporal bone. Intratemporal facial nerve injury that arises along its entire course with consequential impairment or loss of cochlea-vestibular function may require a translabyrinthine decompression.
Complications
As with any surgical procedure, there are some risks involved with the decompression of the facial nerve. These risks include, but are not limited to, post-operative conductive and sensory hearing loss as well as epidural bleeding, edema within the temporal lobe and meningitis among others. Uncontrolled bleeding is one of the most serious complications that can arise during the surgery. In addition to this, patients may suffer headaches and inadvertent injury to other cranial nerves.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1516452/pdf/califmed00056-0033.pdf
- http://onlinelibrary.wiley.com/doi/10.1288/00005537-197906000-00006/abstract;jsessionid=B7F65862B896F5EAD2E175C5833411C1.f04t03
- https://www.ncbi.nlm.nih.gov/pubmed/6834955
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4329040/
- Ballenger's Otorhinolaryngology (16 ed.). BC Decker Inc. pp. 489–516.
Further Reading
- All Paralysis Content
- Paralysis – What is Paralysis?
- What Causes Paralysis?
- What is Tetraparesis?
Last Updated: Aug 23, 2018

Written by
Dr. Damien Jonas Wilson
Dr. Damien Jonas Wilson is a medical doctor from St. Martin in the Carribean. He was awarded his Medical Degree (MD) from the University of Zagreb Teaching Hospital. His training in general medicine and surgery compliments his degree in biomolecular engineering (BASc.Eng.) from Utrecht, the Netherlands. During this degree, he completed a dissertation in the field of oncology at the Harvard Medical School/ Massachusetts General Hospital. Dr. Wilson currently works in the UK as a medical practitioner.
Source: Read Full Article
