Arthritis is a general term to describe inflammation of the joints. However, there are different types of arthritis, including osteoarthritis (OA) and rheumatoid arthritis (RA).
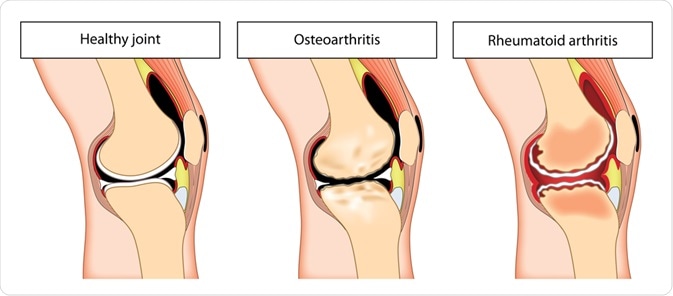 Image Credit: Blamb / Shutterstock.com
Image Credit: Blamb / Shutterstock.com
Degenerative disease vs. autoimmune disease
OA is defined by cartilage degeneration and bone breakdown at the joint surfaces. This causes synovial fluid within the joint to increase, leading to swelling, stiffness and pain. However, pain also occurs spontaneously and unpredictably, and the relationship between the disease process and the symptoms is unclear as of now.
RA is an autoimmune process manifested in the joints but also in the other parts of the body, like the eyes, heart, lungs, and skin. The immune system reacts to one or more of the body’s tissues without obvious cause, triggering inflammation and damage to the cartilage and underlying bone. The synovial membrane is inflamed and thickened and is called the pannus. The result is progressive bone damage and joint deformity, most typically in the small joints of the hands and feet.
Prevalence
Osteoarthritis is the most common forms of arthritis, about 10 times as common as RA. Osteoarthritis affects an estimated 27 million Americans, whereas rheumatoid arthritis affects 1.3 million. Both conditions are more common in women; 75% of persons with RA are women.
Age of onset
RA affects people between the ages of 30 and 60, but can start at any age, including childhood. OA generally starts later in life and is more common in older adults.
Causes
OA is the result of aging and risk factors, including injury, repetitive stress on joints, family history, and genetics. The joint cartilage cells appear to lose their mature characteristics and become more like embryonic cells that convert cartilage into bone in fetal life.
With RA, no specific cause is known despite research into genetic and ethnic factors. Since RA affects people of all backgrounds, it is difficult to determine one specific cause.
However, scientists think that when early cartilage damage occurs, it triggers activation of synovial cells that behave like fibroblasts. These then cause a vicious cycle of cartilage destruction by invading it and releasing breakdown chemicals associated with inflammation.
In both cases, as cartilage breaks down it releases soluble chemicals in the matrix, that interacts with the cartilage cells.
Symptoms
Clinical course
Rheumatoid arthritis symptoms generally have a rapid onset over a short period of time; for example, a matter of weeks. Osteoarthritis symptoms develop slowly and gradually worsen over many years.
Duration of stiffness
OA joint stiffness and pain are a result of inactivity or overactivity, and not an autoimmune process. Further, pain and stiffness are often worse at night for people with OA, and morning stiffness lasts less than 30 minutes. OA pain is sometimes increased after exercise and pressure on joints, and rubbing, grating or crackling noises are heard when afflicted joints are moved. Swelling tends to be mild if it is present.
With RA, With RA joint symptoms include morning stiffness for over one hour, symmetrical joint pain, deformity and restriction of movement at joints.
Joints affected
OA typically affects the larger joints, such as in a knee, hip or shoulder. Asymmetrical OA is common, but OA can also cause pain to the spine and hip. RA is a systemic disease, usually affecting 3 or more joints on both sides of the body symmetrically, most often the small joints of the wrists, fingers, knees, feet and ankles. Over time, affected joints may lose their range of motion and become deformed
Systemic involvement
With OA, the joint symptoms are prominent and no whole-body symptoms are reported. In RA, the person typically feels ill and tired in addition to the joint pain. Non-joint symptoms are often present, including fever, chest pain while breathing, dry eyes and mouth, fatigue and malaise, nodules on under the skin when the disease is more severe, numbness, tingling and/or burning of hands and feet, and sleep problems.
Diagnosis
OA is diagnosed with imaging tests, including x-rays and MRIs, looking for joint damage and cartilage involvement. Blood tests (anti-citrullinated protein antibody) are done to confirm RA. A physical examination will pick up tenderness, redness, swelling and range of motion in the affected joints.
RA can be hard to diagnose because it may start out with subtle symptoms, such as achy joints or some morning stiffness, and those early symptoms can mimic other diseases like OA. Early on, there is no single test to confirm an RA diagnosis. Rather, doctors will make the diagnosis by looking at the patient's symptoms, blood work, x-rays, and results from the physical exam. The X-ray of the hand may show erosions or decalcified areas.
Treatment
The goal of treatment for both RA and OA is to reduce pain, manage symptoms and halt further joint damage. Non-steroidal anti-inflammatory drugs (NAIDs) are prescribed to help with pain and to reduce swelling.
Osteoarthritis is also sometimes treated with steroid injections into affected joints for pain relief and restoration of function. Physical therapy helps to stabilize and strengthen joints. Heat, rest, weight reduction, and massage also help with pain management.
People with RA need stronger oral steroids such as prednisone to manage inflammation. They also use medications that prevent joint destruction and halt disease progression, including biologics and disease-modifying anti-rheumatic drugs, or DMARDs (methotrexate). Biologics and DMARDs are known for their effectiveness, as well as their increased risk for side effects and infections.
Outlook
There is no cure for OA or RA. With a proactive approach to lifestyle, making appropriate changes in the way things are done, and keeping physically active, with medications as prescribed during regular checkups, OA patients can experience significant relief in pain and mood.
The outlook for RA is unpredictable, and numerous complications can arise from this autoimmune disease. And because RA is different for each patient, there is no general prognosis. However, many new treatments have been developed over the last 30 years that aim to lower inflammation, help with pain, prevent joint damage and halt the disease's progress. As a result, people with RA have a much better quality of life today than they did two decades ago.
Sources
- Mayoclinic.org. (2019). Rheumatoid arthritis. www.mayoclinic.org/…/ovc-20197388
- Mayoclinic.org. (2019). Osteoarthritis. www.mayoclinic.org/…/ovc-20198248
- Rheumatology.org. (2019). Rheumatoid Arthritis. www.rheumatology.org/…/Rheumatoid-Arthritis
- Uwhealth.org. (2019). Comparing rheumatoid arthritis and osteoarthritis. www.uwhealth.org/…/aa19377.html
- Cartilage damage in osteoarthritis and rheumatoid arthritis—two unequal siblings. Thomas Pap & Adelheid Korb-Pap. Nature Reviews Rheumatology, volume 11, pages 606–615(2015). https://doi.org/10.1038/nrrheum.2015.95. https://www.nature.com/articles/nrrheum.2015.95#article-info
<<
- All Arthritis Content
- What is Arthritis?
- Types of Arthritis
- Arthritis Treatment
- Arthritis History
Last Updated: Dec 16, 2019

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
