Epilepsy is a common neurological disorder that affects 65 million people around the world. Despite being so common, it is generally not well understood and around one-third of those afflicted cannot control their condition with medication.
One of the emerging ways to deal with epilepsy is to induce seizures in a controlled manner, which has shown promise as a therapeutic method.
Image Credit: Kateryna Kon/Shutterstock.com
How can stimulated seizures help?
Most of the time, epilepsy is treated with medication. However, when drug treatments fail, surgery is usually carried out. For surgery to be successful, physicians need to be able to pinpoint where seizure activity originates from and record how the seizure spreads and affects the patient.
This typically involves hospitalization and observation for an extended period, typically at around two weeks, but stimulated seizures can speed up this process and improve surgical outcomes.
The improved surgical outcome comes from an improved understanding of the location of the seizure onset zone. Specifically, using stimulated seizures to pinpoint the origin of epileptic seizures improved surgical outcomes by around 6%, from 57% to 63%.
In addition to being used as a more diagnostic tool to prepare for surgery, stimulated seizures have been used as a treatment method.
For some patients, seizures continue even after surgery. To stop uncontrolled seizures, other types of induced seizures or/and more invasive intracranial stimulation has been used to some success.
More invasively, deep brain stimulation of the anterior thalamus and the hippocampus led to significant reductions in the frequency of seizures. However, seizure frequency was only reduced by 17.4% and 28.1% respectively.
Complete termination of seizures or a 50% reduction in seizure frequency could not be attained. Treatment was carried out for one to three months before effects were seen.
One of the more common seizure stimulation methods for therapeutic purposes is vagus nerve stimulation. This is also used when drugs are ineffective and are used to treat focal or partial seizures.
This type of stimulation has the advantage of being more directly user-operated – this means that if a patient with a vagus nerve stimulation implant can feel a seizure happening, they can swipe a magnet over their implant. This has been known to help stop the seizure.
How are seizures stimulated?
The stimulation used in preparation for surgery is cortical stimulation. This method uses electrodes to stimulate the brain during intracranial electroencephalography (EEG).
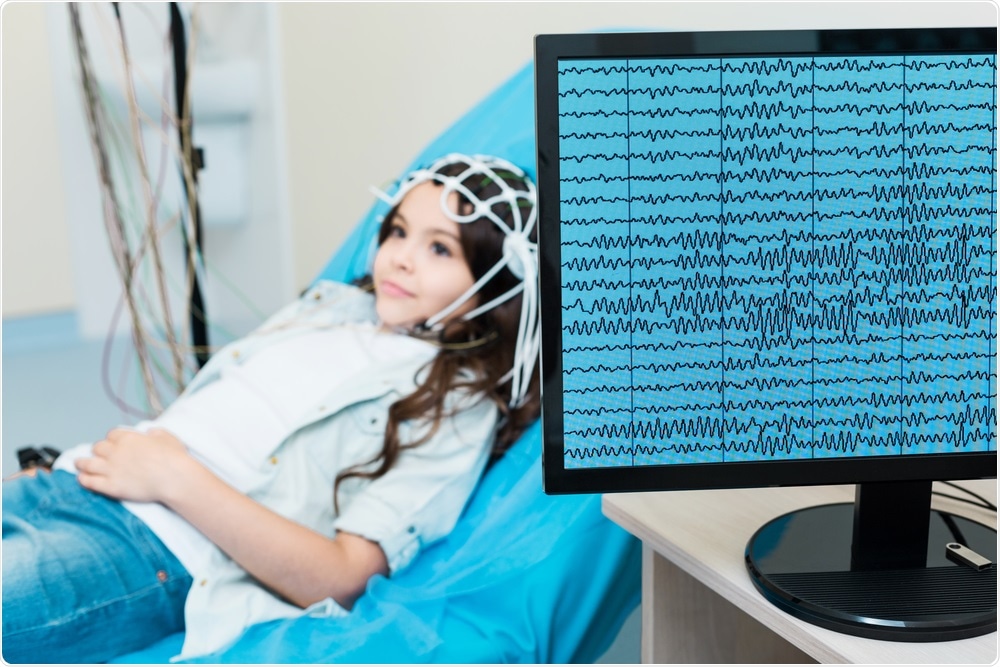
Image Credit: YAKOBCHUK VIACHESLAV/Shutterstock.com
This allows for localization of the brain’s functional areas, in addition to producing seizure activity that can help pinpoint the origin of the seizure.
Deep brain stimulation is more invasive than cortical stimulation. It involves the implantation of an electrode in the brain, as well as the implantation of a pulse generator.
While the exact way deep brain stimulation works is not known, it is believed that the continuous current emanating from the electrodes inhibits targeted brain structures, at least functionally.
The location of the electrodes can also influence their effect, as they can be placed, for example, in the hippocampus to inhibit the epileptic seizures’ onset region or in the thalamus to inhibit its propagation.
Vagus nerve stimulation is not dissimilar to cortical stimulation. The difference is that vagus nerve stimulation operates via the vagus nerve, sending regular mild electrical pulses.
While an implant is required, the implant is placed in the chest rather than in the brain. The device is then wired to the vagus nerve in the neck, which delivers the electrical pulses to the brain.
Limitations of using seizures
One of the main limitations of using seizures for therapeutic and diagnostic purposes is that they cannot always be induced. In a controlled study that used cortical stimulation to prepare for surgery, it was found that seizures could not be induced in 43% of patients in the study.
It is theorized that the reason seizures may not be successfully induced could be because the electrodes were placed in areas with a high neuronal threshold, which the electrodes could not reach to induce seizures.
Other factors, such as time since last seizure, also influenced whether induction was successful, with a 24-hour window or longer being the most successful.
Another big limitation of studies on epilepsy and responses to epileptic treatments is limited to sample sizes. A systematic review on the use of stimulated seizures to help manage epilepsy found that hippocampal deep brain stimulation reduced seizure frequency, but the sample size was too limited for any conclusions of its safety and tolerability to be made.
The same systematic review also found signs of selective reporting in the studies used. Out of the twelve randomized control trials it used in the study, four showed signs of selective reporting. This can be an indicator of weaker reliability of some of the studies on epileptic treatment via stimulated seizures.
Sources
- Cuello Oderiz, C. et al. (2019). Association of cortical stimulation-induced seizure with surgical outcome in patients with focal drug-resistant epilepsy. Journal of the American Medical Association. https://doi.org/10.1001/jamaneurol.2019.1464
- Sprengers, M. et al. (2017). Deep brain and cortical stimulation for epilepsy. Cochrane Database Systematic Reviews. https://doi.org/10.1002/14651858.CD008497.pub3
- Shafer, P.O., and Dean, P.M. (2018). Vagus nerve stimulation (VNS). www.epilepsy.com/…/vagus-nerve-stimulation-vns
Further Reading
- All Epilepsy Content
- What is Epilepsy?
- Epilepsy Classification
- Epilepsy Epidemiology
- Epilepsy Pathophysiology
Last Updated: Apr 27, 2020

Written by
Sara Ryding
Sara is a passionate life sciences writer who specializes in zoology and ornithology. She is currently completing a Ph.D. at Deakin University in Australia which focuses on how the beaks of birds change with global warming.
Source: Read Full Article
