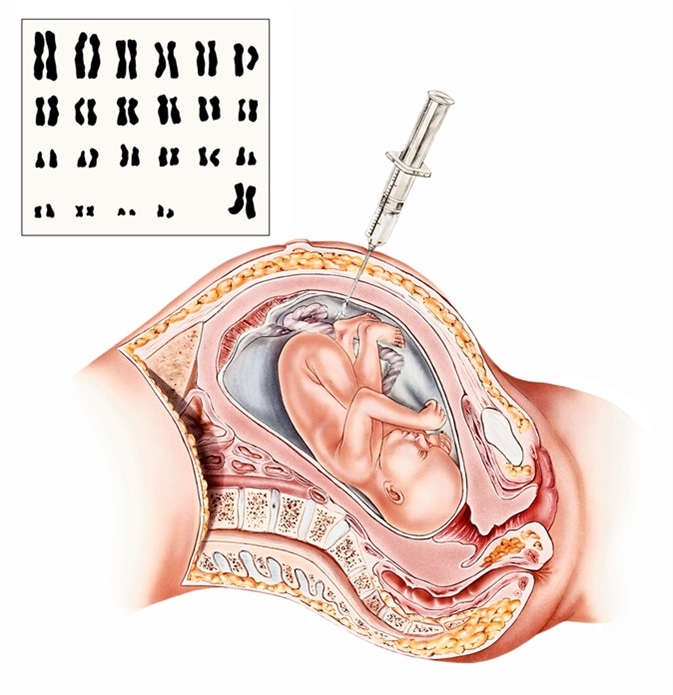
Amniocentesis is a diagnostic procedure in which a small amount of amniotic fluid is removed from the sac of amniotic fluid around the baby inside the uterus, to test for certain chromosomal anomalies and other genetic defects. This fluid is meant to protect and nourish the baby and is vital for its proper development.
Amniocentesis Indications
Amniocentesis should not be treated as a routine procedure because of its associated risks. Some specific indications for doing an amniocentesis include:
- Genetic amniocentesis: This is the most common indication for amniocentesis and is done when the healthcare provider thinks it will be beneficial in managing the pregnancy further or will change the decision of the parents to continue the pregnancy. Testing is carried out for chromosomal defects such as Down syndrome or other trisomies, especially in
- women with a personal or family history of such anomalies
- if they are older than 35 years of age at the time of conception
- if other prenatal screening tests were positive or borderline
- fetal ultrasound scanning was abnormal in a way that suggests genetic defects
- Testing fetal lungs for maturity if a baby is to be delivered before term (between 32 and 39 weeks of pregnancy) for non-emergency situations
- Testing for fetal infection or for assessing fetal hemoglobin levels, when the mother is sensitized against the fetal red cells, causing them to be destroyed by maternal antibodies passing into the fetal circulation
- Removal of excessive amniotic fluid if it is causing maternal distress or medical complications.
Contraindications
Amniocentesis may be contraindicated if the mother is HIV positive, has hepatitis B, or hepatitis C, which could be vertically transmitted by amniocentesis.
Risks
While the procedure is generally safe, its risks include:
- Amniotic fluid leakage: this is uncommon, usually small, and self-limited (stops within a week), with no permanent negative fallout on the pregnancy
- Miscarriage: the risk of losing the baby is about 0.6%, and is higher when it is done before 15 weeks
- Needle injuries: while occasional puncture injuries may occur to the baby because of movement into the path of the needle, serious injuries are very rare
- Rh isoimmunization: This is a complication caused by the contamination of the mother’s Rh-negative blood by the fetal Rh positive red cells, causing immunization. The antibodies produced as a result, cross the placenta and cause clumping and destruction of the fetal red cells, resulting in severe fetal anemia and even death. This is prevented by Rhogam injections following the procedure. Maternal blood is also tested to screen for these isoantibodies.
- Infection: sometimes, amniocentesis may cause infection within the uterus. Some infections may also be transferred to the fetus during the procedure, such as hepatitis C, HIV, or toxoplasmosis.
Warning Signs
Following the procedure, some situations should cause concern and prompt an immediate evaluation:
- Bleeding from the vagina or the needle puncture
- Amniotic fluid leaking from the vagina or needle puncture
- Fever or chills
- Severe abdominal pain
- Changes in fetal activity past 20-24 weeks
Sources
- www.mayoclinic.org/tests-procedures/amniocentesis/about/pac-20392914
- https://www.nhs.uk/conditions/amniocentesis/what-happens/
- www.urmc.rochester.edu/…/content.aspx
- my.clevelandclinic.org/…/procedure-details
Further Reading
- All Amniocentesis Content
- Amniocentesis Procedure
Last Updated: Feb 26, 2019

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
