Seroconversion is the transition from the point of viral infection to when antibodies of the virus become present in the blood. Given that many diagnostic tests use the presence of antibodies to infer illness, understanding seroconversion becomes a very important part of immunology and virology.
.jpg)
Image Credit: Kateryna Kon/Shutterstock.com
Why is determining seroconversion important?
Antibodies can be important for diagnosing disease in several viral contexts, such as with HIV. In many cases, accurate diagnosis of COVID-19 is done by nucleic acid tests. However, there is some dispute over this, with some research indicating that detection of seroconversion can detect virus-specific antibodies despite negative nucleic acid tests.
Either way, determining seroconversion can be important for understanding the immune response, infection rates, and identification of potential serum donors.
Understanding all three aforementioned benefits of studying seroconversion is critical for understanding disease proliferation and spread. For example, information on the rate of infection is needed to determine the infection fatality rate with any accuracy.
Understanding the seroconversion in a quantitative manner can allow for the detection of individuals who have strong antibody responses to viruses, and can, therefore, be donors. Similarly, studying seroconversion can aid in understanding which antibody responses are associated with protection from the virus in question.
Seroconversion is not limited to clear cases of infection. Asymptomatic patients can also undergo seroconversion. Similarly, detection of seroconversion does not mean antibodies are present for an indefinite amount of time, nor that all individuals with a disease will undergo seroconversion.
In the case of COVID-19, current research indicates that the production of disease-specific antibodies, or the completion of seroconversion, is completed within 17-19 or 20-22 days of the onset of symptoms, depending on the antibody in question. The median for undergoing seroconversion for COVID-19 immunoglobin G and M (IgG and IgM) is 13 days after symptoms appear.
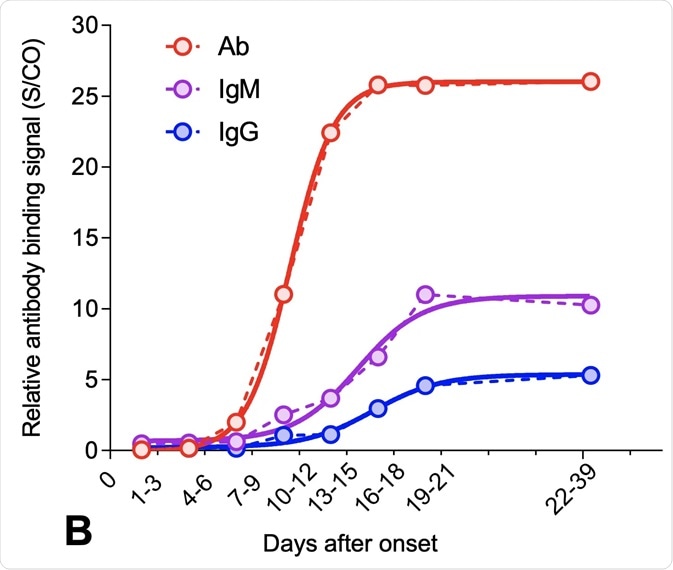
Image Credit: AssayGenie
Seroconversion and infectiousness
In most diseases, infectiousness is at its highest before seroconversion. This is true for HIV, where most seroconversion research has focused, but there is also evidence that this is occurring in SARS-CoV-2. Certain cases also indicate that virus shedding can continue after seroconversion.
While the research on COVID-19 is extensive and mostly very new, the importance of seroconversion is highlighted in many papers. Where viral shedding continues past seroconversion, there are implications that the contagious period is extended by as much as a week after clinical recovery.
Similar results have been found for asymptomatic patients. This can be very damaging for infectious spread and for developing containment strategies.
While seroconversion and the presence of antibodies can, in some diseases, confer immunity from re-infection, this may not always be the case. For example, there is so far not enough data to accurately determine whether seroconversion of COVID-19 leads to protection from re-infection.
The basic reproduction number (R0) indicates how contagious a disease is. Studies on seroconversion and cross-reactivity have shown that when testing for seroconversion, there is little or no cross-reactivity from other human coronaviruses.
This indicates that humans are ‘serologically naïve’ to COVID-19, meaning it has not been encountered before (unlike other viral diseases like influenza). This naivety to COVID-19 can be a contributing factor to the disease’s relatively high R0 number.
How is seroconversion detected?
Seroconversion is detected based on the presence of antibodies. However, different diseases can trigger different types of antibodies. For example, for COVID-19, there have been documented cases of seroconversion of immunoglobin G and M (IgG and IgM, respectively). There can also be different combinations of seroconversion occurring.
In a study of 26 COVID-19 patients, nine patients had synchronous seroconversion of IgG and IgM, seven patients had IgM seroconversion before IgG seroconversion, and ten patients had seroconversion of IgM later than that of IgG.
One way in which seroconversion can be detected is via a replication-competent virus, but this process can take several days and requires strict biosafety regulations. Other methods, which are more recently developed, include the use of traditional ELISAs in combination with pseudotyped viral particle-based entry assays. This type of method does not need to involve live viral particles, and therefore has fewer strict regulations involved and can be carried out easier.
Sources
- Liu, W.D., Chang, S.Y., Wang, J.T., Tsai, M.J., Hung, C.C., Hsu, C.L., Chang, S.C., 2020. Prolonged virus shedding even after seroconversion in a patient with COVID-19. Journal of Infection, In press.
- Amanat, F., Stadlbauer, D., Strohmeier, S., Nguyen, T., Chromikova, V., McMahon, M., Jiang, K., Arunkumar, G., Jurczyszak, D., Polanco, J., Bermudez-Gonzalez, M., Kleiner, G., Aydillo, T., Miorin, L., Fierer, D., Lugo, L., Kojic, E., Stoever, J., Liu, S., Cunningham-Rundles, C., Felgner, P., Moran, T., García-Sastre, A., Caplivski, D., Cheng, A., Kedzierska, K., Vapalahti, O., Hepojoki, J., Simon, V. and Krammer, F., 2020. A serological assay to detect SARS-CoV-2 seroconversion in humans. Nature Medicine, In press.
- Long, Q., Liu, B., Deng, H., Wu, G., Deng, K., Chen, Y., Liao, P., Qiu, J., Lin, Y., Cai, X., Wang, D., Hu, Y., Ren, J., Tang, N., Xu, Y., Yu, L., Mo, Z., Gong, F., Zhang, X., Tian, W., Hu, L., Zhang, X., Xiang, J., Du, H., Liu, H., Lang, C., Luo, X., Wu, S., Cui, X., Zhou, Z., Zhu, M., Wang, J., Xue, C., Li, X., Wang, L., Li, Z., Wang, K., Niu, C., Yang, Q., Tang, X., Zhang, Y., Liu, X., Li, J., Zhang, D., Zhang, F., Liu, P., Yuan, J., Li, Q., Hu, J., Chen, J. and Huang, A., 2020. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nature Medicine, In Press.
Further Reading
- All Coronavirus Disease COVID-19 Content
- What Mutations of SARS-CoV-2 are Causing Concern?
- What is the Clinical Impact of COVID-19 on Cancer Patients?
- Can Pets Get COVID-19?
- An Overview of the SARS-CoV-2 Vaccines
Last Updated: Jun 10, 2020

Written by
Sara Ryding
Sara is a passionate life sciences writer who specializes in zoology and ornithology. She is currently completing a Ph.D. at Deakin University in Australia which focuses on how the beaks of birds change with global warming.
Source: Read Full Article
