- Body mass index (BMI) has long been used as a tool for weight management and intervention, but experts say it has many flaws.
- They say waist-to-hip ratio may be a more accurate indicator of risk of mortality from all causes.
- They add that waist-to-hip ratio may be a more useful tool in healthcare interventions.
Waist-to-hip ratio may be a better tool for determining weight management than body mass index (BMI), according to a new study.
Research published this week in the journal JAMA Network Open reports that waist-to-hip ratio may be more useful than BMI in determining health risks and medical interventions.
For their study, the researchers examined data from 387,672 participants based in the United Kingdom. They compared data on BMI, fat mass index, and waist-to-hip ratio.
“Compared with BMI, [waist-to-hip ratio] had the strongest, most robust, and consistent association with all-cause mortality and was the only measurement unaffected by BMI. Current WHO recommendations for optimal BMI range are inaccurate across individuals with various body compositions and therefore suboptimal for clinical guidelines,” the researchers wrote.
“Future research is needed to explore whether using WHR as the primary clinical measure of adiposity (body fat) would help to improve long-term health outcomes in distinct patient populations compared with BMI. Our results provide further support to shift public health focus from measures of general adiposity, such as BMI, to adiposity distribution using [waist-to-hip ratio],” the study authors added.
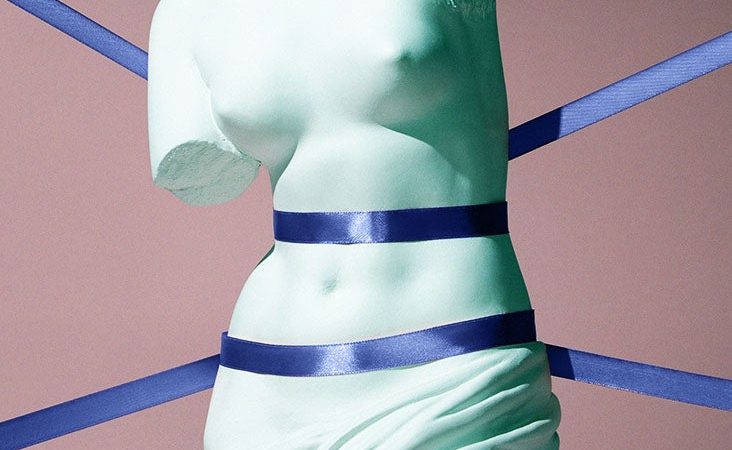
What is waist-to-hip ratio?
Waist-to-hip ratio is the circumference of the waist divided by the circumference of the hip.
In both men and women, a waist-to-hip ratio of 1.0 or above is considered at risk for conditions such as heart disease.
Those who carry excessive fat around their midsection may be at greater risk of developing type 2 diabetes, coronary heart disease, and high blood pressure.
BMI is a commonly used tool for weight management and is calculated by dividing a person’s weight in kilograms by their height in meters squared.
The problem with BMI
Experts say BMI can be a problematic tool.
“BMI historically has been ‘the’ tool used in weight management in doctor’s offices, hospitals, etc. Even to this day it is still used. That’s because it is extremely easy to calculate. All you need is height and weight. However, BMI is fraught with problems, one of them is that you can have a weight lifter with 8% body fat with a BMI of 35 and you can have someone who has 35% body fat with the same BMI. It’s nonspecific,” said Dana Hunnes, PhD, a senior clinical dietitian at the UCLA Medical Center in Los Angeles who was not involved in the new study.
“Waist-to-hip ratio does do a better job of capturing visceral fat, mid-body fat, waist fat, the fat that is most harmful in terms of all-cause and cause-specific mortality,” Hunnes told Medical News Today. “So yes, given that this is a better measure, surrogate for adiposity in general and adiposity distribution, I do think that we should be using it more often.”
Despite the flaws of the BMI, experts note it is still a commonly used tool.
“It has a very significant amount of flaws in it… but it is a useful tool,” said Dr. Dan Azagury, the section chief of Minimally Invasive and Bariatric Surgery at Stanford University in California who was not involved in the study.
“It’s still a useful tool for multiple reasons,” he told Medical News Today. “One is, it is pretty deeply ingrained in a lot of the things that we use… The guidelines from the [Food and Drug Administration] and the [National Institutes of Health] around management of obesity are still around BMI.”
“What your insurance will pay, what treatment they will pay for is based on BMI,” Azagury added. “So while I agree that it’s flawed, it’s here and it’s so widely used that we’re probably going to have to live with it for a lot longer.”
Risks of being overweight or having obesity
According to the Centers for Disease Control and Prevention (CDC), people who are overweight or have obesity are at an increased risk for a number of diseases and health conditions.
This includes death from all causes, hypertension, stroke, mental illness, sleep apnea, gallbladder disease, osteoarthritis, breathing problems, low quality of life, trouble with physical functioning, and type 2 diabetes.
“The higher our adiposity (the more fat we have in our bodies, and specifically, the more visceral/mid-body fat we have), the greater is our risk of dying from any cause and from cause-specific (cardiovascular disease, cancer). The higher our body fat, the more likely it is we will die sooner,” Hunnes said.
“Due to the associations/relationships between all-cause and cause-specific mortality and adiposity, it’s important to have a reliable surrogate measure of adiposity. This is used as an independent predictor of all-cause and cause-specific mortality,” she added.
In the United States, nearly 74% of adults aged 20 and over are classified as overweight or obese.
In 2019 dollars, the CDC estimated that the annual cost related to obesity is $173 billion.
Stopping the stigma of obesity
Azagury argues that while having a reliable tool with which to measure and manage weight is important, this is only part of the puzzle in helping those who are overweight or have obesity.
“The challenge still is that the vast majority of patients do not come and seek medical help to tackle their obesity. And when they do, they’re still faced many times by stigma from their provider,” he said.
“Right now, we don’t even have an opportunity to treat most of the people that actually would benefit from treatment. What we need to tackle is the stigma around obesity, and that it is a disease that needs to be treated, and that patients who have obesity should not be ostracized,” Azagury added.
Source: Read Full Article