Systemic lupus erythematosus (SLE) is an autoimmune disease in which the immune system attacks the body’s own tissues, causing widespread inflammation and damage in the affected organs. It can affect the joints, skin, brain, lungs, kidneys, and blood vessels. Asian SLE patients suffer from more severe disease and damage compared to patients in western countries.
In Singapore, the prevalence of childhood SLE has been reported to be 14.2 per 100,000 children, while that of adult SLE is 40 per 100,000 adult population. Cognitive dysfunction is common in patients with SLE. Earlier studies have shown that 25% of SLE patients were found to have cognitive dysfunction, compared to 7.3% in age- and gender-matched healthy individuals. Common cognitive dysfunction demonstrated by SLE patients includes impairment of simple reaction time, sustained and selected attention, memory search, working memory, and short-term memory for learnt associations, which result in reduced health-related quality of life and a negative impact on vocational capability.
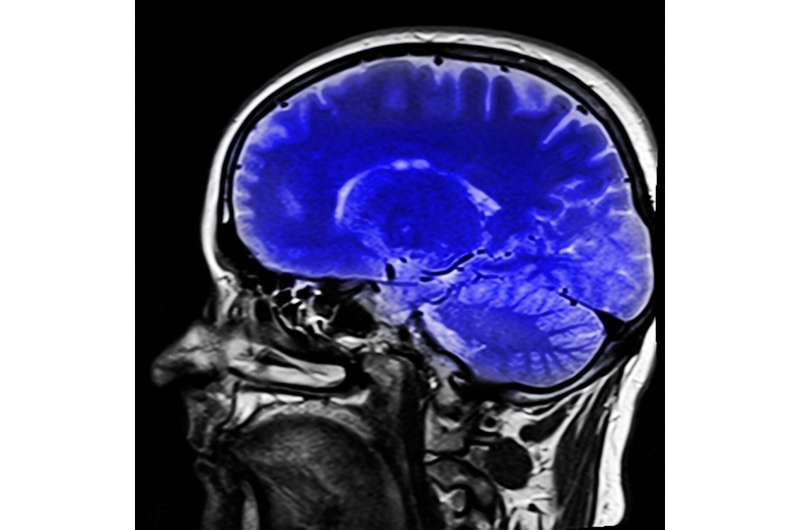
The neural mechanism leading to cognitive dysfunction in patients with SLE remains unknown. Researchers at the NUS Yong Loo Lin School of Medicine attempted to unravel such mechanisms by adopting non-invasive diffusion magnetic resonance imaging (MRI) to study the brains of SLE patients, particularly the white matter, coupled with computerized neuropsychological assessment. White matter lies beneath the gray matter cortex in the human brain and comprises millions of bundles of nerve fibers that transmit signals to different brain regions.
Led jointly by Associate Professor Juan Helen Zhou, from the Centre for Sleep and Cognition and Deputy Director for the Centre for Translational Magnetic Resonance Research at NUS Medicine, and Associate Professor Anselm Mak, a clinician scientist with the Division of Rheumatology at the Department of Medicine, the group investigated free water changes in white brain matter in SLE. This comprises water molecules surrounding white matter in the brain that are able to diffuse unhindered.
In the paper published in Rheumatology, they compared the free-water signals in SLE patients without clinically overt neuropsychiatric manifestations with a group of matched healthy participants using the novel free water diffusion MRI technique. They discovered that patients with SLE had significantly higher white matter free water than their healthy counterparts, suggesting possible microvascular degradation and/or inflammation. Such increases in free water were significantly related to cognitive dysfunction, especially sustained attention, as well as cumulative dosage of medical steroids.
“The clinical implications of the study would indicate to physicians that steroids should be judiciously prescribed, aiming for the lowest possible dose for the shortest possible duration. While systemic use of steroids will continue to be the mainstay of treatment for moderate to severe SLE-related inflammation, there are other therapeutic options that could produce similar results: these should be considered first in order to reduce steroid use or shorten the necessary course,” said Assoc Prof Anselm Mak.
He also added that there are other SLE manifestations that could be symptomatically treated without the prescription of steroids. For example, non-steroidal anti-inflammatory drugs could be used for milder inflammation, topical treatment for hair loss and topical analgesics for oral ulcers.
SLE patients on long-term steroid treatments should also be regularly assessed and monitored for cognitive dysfunction. The researchers noted that the use of the Automated Neuropsychiatric Assessment Matrix (ANAM), which has been validated for use in adult and pediatric SLE patients, is an efficient and effective tool for these regular evaluations.
Source: Read Full Article
