Many Americans became amateur data scientists during the pandemic, tracking local rates of infection or vaccination to help them decide what activities may or may not be safe. UChicago researchers saw an opportunity to dig deeper: By using county-level data, they found that different demographic groups are vulnerable in different ways—often depending on their geographic location.
What they discovered was that not all of a particular race or ethnic population in the U.S. is impacted by the same factors, or face the same COVID-19 outcomes. By identifying associations between COVID mortality and social determinants of health, the research team uncovered the specific ways that place has shaped how people experience the pandemic.
“We know it’s not just different demographics alone,” said Susan Paykin, a senior research manager at UChicago’s Center for Spatial Data Science. “It’s the structural, economic and social factors that define those places that are influencing higher death rates and case rates.”
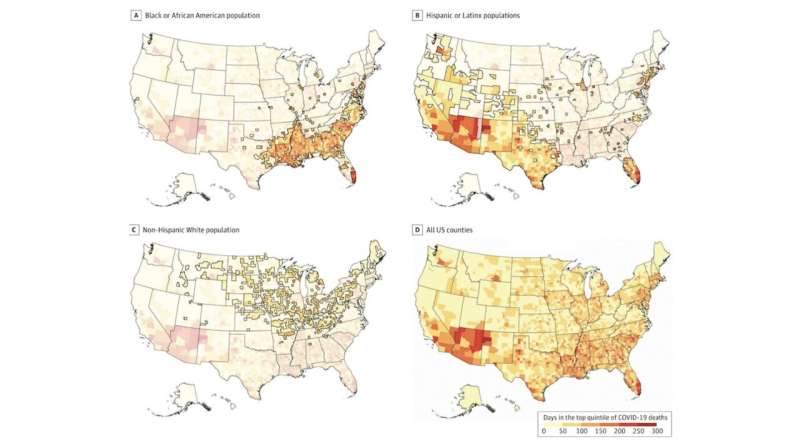
The findings, published in JAMA Network Open, came from a cross-sectional study of 3,142 counties in 50 U.S. states and the District of Columbia—focusing on Black or African American, Hispanic or Latinx, and non-Hispanic White populations. The team looked at those different groups and their various social factors and whether they differed or were similar across urban, rural and suburban counties.
According to the study, Black or African American groups with high mortality rates—particularly in the Southeast—were more vulnerable due to low socioeconomic status, high income inequality, limited access to quality health care, and severe housing problems. White populations who experienced high mortality rates—most often in the rural Midwest—are located mostly in counties with a high percentage of older populations, and who have limited access to quality health care.
The team was made up of spatial data scientists and public health researchers who are part of the Healthy Regions and Policies Lab at UChicago’s Center for Spatial Data Science. This team works on the U.S. COVID Atlas, a free and open-source data visualization tool that connects COVID data and community indicators.
The team observed that different minority groups were experiencing disproportionately high mortality rates during the pandemic—but the available data from the CDC doesn’t show much granularity below the state level as it relates to race and ethnicity.
“Different groups are vulnerable in different ways,” said Qinyun Lin, a postdoctoral scholar at the center and the first author of the study. “In Hispanic groups, we found that many have high mortality rates in urban areas. We found those who are most vulnerable are in areas associated with a high percentage of working-age people and low insurance rates and severe housing problems.”
“Our research looks at COVID mortality rates, specifically the highest mortality rates in the first year of the pandemic,” said Paykin. “Then we look at how that matches with where different race and ethnicity groups live and we try to get at where high mortality rates disproportionately impacted different groups. And what social structural factors are associated with those outcomes?”
The researchers relied on two data inputs in particular. One was county-level COVID mortality data from the CDC, focused on the first year of the pandemic. They used county-level data from the U.S. Census Bureau’s American Community Survey and County Health Rankings & Roadmaps, which included demographics and community contextual factors. They looked at community-level variables such as income inequality, the ratio of population to primary care physicians, rates of preventable hospital stays, percentage of severe housing problems, percentage of internet access, and age distribution.
This data was then compared to previous literature on variables that have been shown to be associated with COVID-19 mortality. The team also spoke with their colleagues working on County Health Rankings for further insight.
The researchers are hoping their paper encourages information to be collected at a more granular level and shared freely—not only in the context of the COVID-19 pandemic, but also to have in place for future pandemics or other natural disasters.
“We hope to show how place impacts COVID-19 outcomes,” Paykin said. “These outcomes are not driven by the people themselves, but rather the conditions that define the places in which they live. And that has really important implications for policy and structural changes and how we formulate and begin to prepare for the future and build a culture of health equity in general, for different populations across different communities in the U.S.”
As a next step, the researchers are looking to expand their datasets to include different ethnicities. The only reason they weren’t included in this study was because the level of available data was not large enough for statistically significant summaries. The current study is mainly exploratory and looks at associations. The researchers are also interested in digging deeper into different urban, rural and suburban settings to better understand the structural factors and drivers related to higher COVID mortality and death rates.
Source: Read Full Article
