With more than 330 million documented cases of infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) worldwide since the start of the pandemic, vaccination was initially viewed as the definitive solution to the global crisis caused by coronavirus disease 2019 (COVID-19). However, the emergence of new SARS-CoV-2 variants and strains with markedly higher infectivity has significantly limited the effectiveness of current COVID-19 vaccines.

Study: Functional Status, Mood State, And Physical Activity Among Women with Post-Acute COVID-19 Syndrome. Image Credit: fizkes / Shutterstock.com
Background
Apart from the significant minority of critical and fatal outcomes that occur due to SARS-CoV-2 infection, a large number of patients have reported not feeling well for weeks or months after diagnosis. This phenomenon has been termed post-acute COVID-19 sequelae (PASC). The symptoms of PASC vary from physical ones like breathlessness, extreme fatigue, and sensory changes to mental fog and cognitive impairment.
The long-term impact of PASC is still being examined. However, this condition will likely increase the burden on health services, especially as it has been observed to follow even asymptomatic or mild infection.
Women have been shown to be three or four times as likely to seek treatment for PASC symptoms. Since women are also at higher risk for disability with increasing age as compared to men, the functional sequelae of PASC in this group deserve careful evaluation.
With the implementation of restrictions on interactions between non-household members in spaces outside the home, there has been a significant reduction in physical activity. The magnitude of this change could be, in part, due to the occurrence of PASC, as well as the restrictions in force at the time.
The importance of declining physical activity is the cascading effect on mood states and psychological well-being. Younger females with a lower-than-average income, especially those with multiple illnesses, have been shown to have worse mental health due to the onset of COVID-19.
The current study published on the medRxiv* preprint server attempts to measure the difference in mood, functional status, and leisure-time physical activity.
Study findings
Of the 32 participants included in the current study, about 45% were normal weight; however, over a third were overweight, and one in five were considered to be obese. The median time from symptom onset to enrolment in the study was 85 days. Over 70% of the study participants reported a loss of taste and/or smell, with over half reporting fever and/or cough, while more than 40% described aches in the joints or muscles.
The fever lasted between one and 16 days, whereas the sore throat remained present for two to zero days. Over half of the participants had symptoms at the time of testing and were at a median of 74 days from diagnosis.
Walking self-efficacy is a measure related to the ability to be active and enjoy the normal physical function. The functional status, which was measured by a modified Pulmonary Functional Status and Dyspnea Questionnaire (PFSDQ-M), refers to the degree of fatigue and breathlessness experienced during 10 activities of daily living (ADL). These measures were found to be inversely related to each other.
While walking self-efficacy did not show a significant reduction in the study participants, functional status and leisure-time physical activity showed deterioration in those with a history of SARS-CoV-2 infection. This observation was positively correlated with the increasing workload on the heart due to a raised blood pressure and heart rate.
Mood changes were assessed using the Profile of Mood States (POMS) questionnaire. SARS-CoV-2 participants also reported a greater disturbance in mood. Tension and confusion were higher in these participants in half of the subscales.
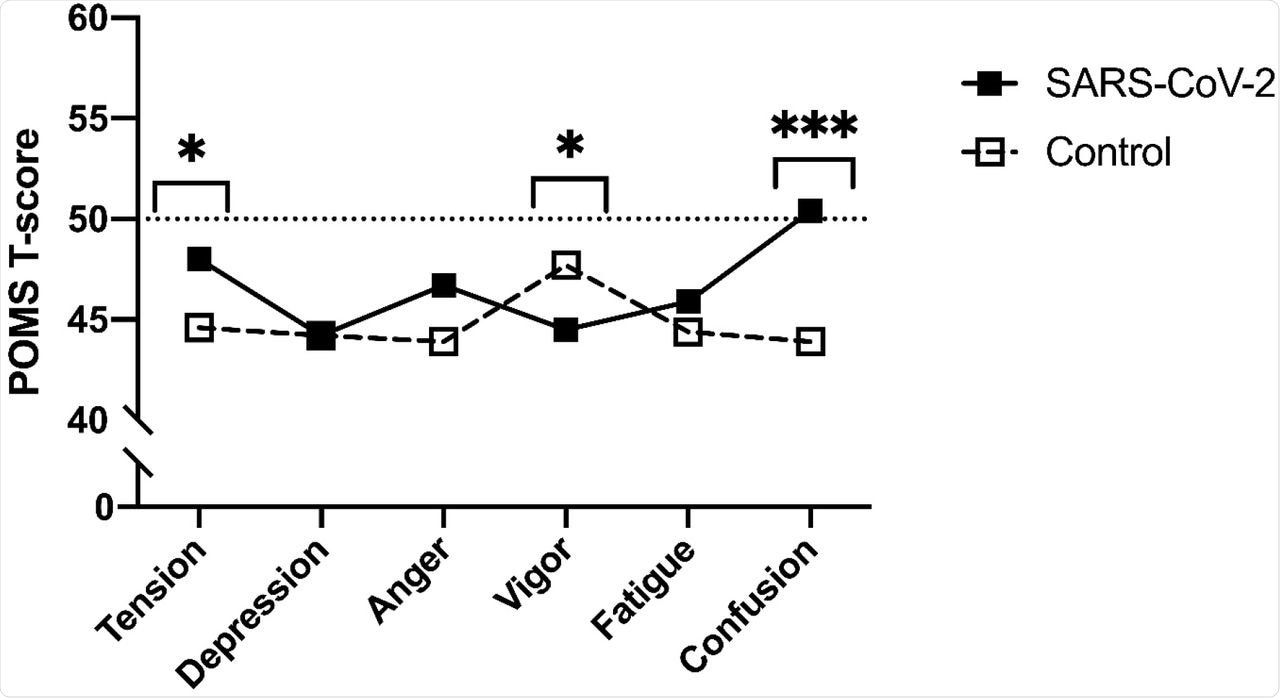
Profile of Mood States (POMS) sub-scale T-scores between SARS-CoV-2 and control participants.
Among individuals with a history of SARS-CoV-2 infection, those who were more symptomatic at disease onset were more likely to experience confusion at the time of the study at all ages and irrespective of the body fat percentage. The functional impairment was also greater with a greater number of days of anosmia or ageusia, was greater among SARS-CoV-2 patients who complained of fatigue and was lower among controls who reported feeling angry.
Asymptomatic patients had higher median walking self-efficacy as compared to symptomatic patients at 100 and 60, respectively. Functional levels were lower in symptomatic patients, with scores of 15 as compared to an average score of five in asymptomatic patients.
Patients who showed a greater cardiac workload showed lower walking self-efficacy, that is, were less likely to be able to be physically active.
Implications
The findings of the current study demonstrate that even after compensating for age, body mass index, smoking history, and cardiovascular or pulmonary disease, there were significant differences in the mood between SARS-CoV-2 and control participants. In fact, individuals with a history of COVID-19 reported a negative mood in over a third of cases, while controls showed a more positive mood.
Individuals with a history of SARS-CoV-2 infection also were more tense and confused, with low vigor. Tension measures were higher in the SARS-CoV-2 group as compared to non-infected women. However, the low levels of vigor were not correlated with fatigue measures.
Earlier coronavirus outbreaks showed negativity of mood and reduction in memory, both during the acute phase and during the recovery phase, among those hospitalized. It is expected, based on the findings of this study, that the same trends may prevail in SARS-CoV-2 patients as well.
The role of PASC as compared to direct viral injury needs to be further elucidated out by more research. In the current study, anosmia and ageusia were associated with a higher percentage of tension and depression, thus leading to the hypothesis that SARS-CoV-2 might travel backward from the peripheral nerves, such as the gustatory and olfactory nerves, to reach the brain.
Acute-phase functional deterioration in SARS-CoV-2 infection extends into the post-acute recovery phase, as shown in this study, even 74 days from diagnosis. The loss of functional status is traceable to breathlessness, fatigue, and muscle or joint pain, along with depression and anxiety, thereby impairing the ability to carry out ADL and eventually leading to reduced personal care and quality of life.
Another explanation is that greater fatigue makes ADL difficult; therefore, ADL may pose a formidable challenge to the symptomatic patient and increase the feeling of tiredness. Further studies should offer more data about how these symptoms fare with time and how they impact social health, mental well-being, and the quality of life in COVID-19 patients.
Increased symptom numbers at the onset of illness may be associated with depression, anxiety, and post-traumatic stress.
“This finding is consistent with process of interoception wherein peripheral (sensory) feedback provides a moment-to-moment updates of the internal bodily environment. This, in turn, has the potential to trigger a maladaptive cycle that can ultimately interfere with activities of daily living.”
Such phenomena are especially disturbing in women who already have higher age-related disability rates, and in whom symptoms tend to persist after SARS-CoV-2 infection. More work must be carried out to formulate targeted measures that can prevent this observed loss of functional status and ability to be physically active.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Carter, S. J., Baranauskas, M. N., Raglin, J. S., et al. (2022). Functional Status, Mood State, And Physical Activity Among Women with Post-Acute COVID-19 Syndrome. medRxiv. doi:10.1101/2022.01.11.22269088. https://www.medrxiv.org/content/10.1101/2022.01.11.22269088v1.
Posted in: Medical Research News | Medical Condition News | Women's Health News | Disease/Infection News
Tags: Anosmia, Anxiety, Blood, Blood Pressure, Body Mass Index, Brain, Coronavirus, Coronavirus Disease COVID-19, Cough, Depression, Disability, Dyspnea, Efficacy, Fatigue, Fever, Gustatory, Heart, Heart Rate, Joint Pain, Mental Health, Mood Disorder, Muscle, Pain, Pandemic, Physical Activity, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Smoking, Sore Throat, Stress, Throat, Tiredness, Walking

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
