An anonymous San Diego resident has become a fascinating example of how the human immune system fights SARS-CoV-2. In a new investigation, scientists from La Jolla Institute for Immunology (LJI) have shown how antibodies, collected from this clinical study volunteer, bind to the SARS-CoV-2 “Spike” protein to neutralize the virus.
Although studies have shown antibodies bound to Spike before, this new research reveals how the original Moderna SARS-CoV-2 vaccine could prompt the body to produce antibodies against the later omicron variants of SARS-CoV-2. The researchers also capture highly detailed, 3D structures of three promising neutralizing antibodies bound to Spike.
This important work shows exactly where Spike is vulnerable to human antibodies—and how future vaccines and antibody therapeutics might exploit these weaknesses. In fact, studies in mice suggest some of these antibodies may help prevent severe cases of COVID-19.
“To blunt the next pandemic and protect people from seasonal re-emergence of this one, we need antibodies of the broadest possible capacity—ones that are not escaped,” says LJI President and CEO Erica Ollmann Saphire, Ph.D., senior author of the new Cell Reports study. “We found those in a vaccinated San Diegan.”
“Studying that person’s immune response in detail uncovered antibodies that are still effective against many omicron variants,” adds LJI Instructor Kathryn Hastie, Ph.D., co-leader of the study and Director of the LJI Antibody Discovery Center. “We now have to figure out how to boost these antibodies that we want over others that are less effective.”
Taking on viral variants
Throughout the pandemic, scientists at LJI have gathered blood samples here in San Diego, and from labs around the world, with the goal of understanding the roles of different immune cells in fighting SARS-CoV-2.
Antibodies are among the immune system’s most elite fighters. These molecules are made by B cells and each antibody has a specific structure meant to bind to a specific target on a pathogen. It’s as if B cells see a bullseye on a pathogen and then go to work making their arrows.
For the new study, the antibodies came from a clinical studies volunteer who received two doses of the Moderna SARS-CoV-2 vaccine. The Moderna vaccine works by prompting the body to make the Spike protein—glimpses of the viral bullseye—so it can begin work on its antibodies and other weaponry against the real virus.
The samples from the study volunteer were collected in early 2021—before the emergence of omicron. That means any antibodies made by the volunteer were a result of vaccination, rather than exposure to omicron.
The SARS-CoV-2 omicron variant emerged in late 2021 and spread quickly. Omicron stood out from other variants because it contained mutations that helped it evade immune cell protection. Many antibodies designed to fight earlier SARS-CoV-2 variants couldn’t hit their mark on omicron.
Finding winning antibodies
Luckily, not everyone produces the same types of antibodies. In fact, the composition of virus-fighting cells and antibodies varies wildly in each person. For the new study, the researchers began with a pool of antibodies from the San Diego volunteer. Like many people who received the first two Moderna vaccine shots, this individual produced a robust pool of antibodies capable of neutralizing the ancestral D614G variant of SARS-CoV-2.
As new viral variants of concern emerged, the researchers tested this pool to see how many antibodies could still bind to the mutated virus.
“We found that this pool of antibodies could also neutralize other variants, such as delta and omicron,” says Hastie.
They found that the subject maintained moderate to high levels of antibodies against beta, delta and omicron lineages BA.1, BA.1.1 and BA.2. Among these surviving antibodies, the researchers uncovered five antibodies that actually decreased the infectivity of BA.1 by more than 85 percent.
The researchers then took these five remaining antibodies through another battery of tests. One antibody, called 1C3, showed promise in blocking part of the infection process (when the virus’s receptor binding domain interacts with human protein ACE2) but only against BA.1 and BA.2 lineages. Another antibody, 1H2, could also neutralize some omicron lineages, but did so in a different way than 1C3. Meanwhile, antibody 2A10 was reactive to all SARS-CoV-2 omicron lineages tested, including those that are most common now: XBB and BQ1.
Mapping out antibody targets
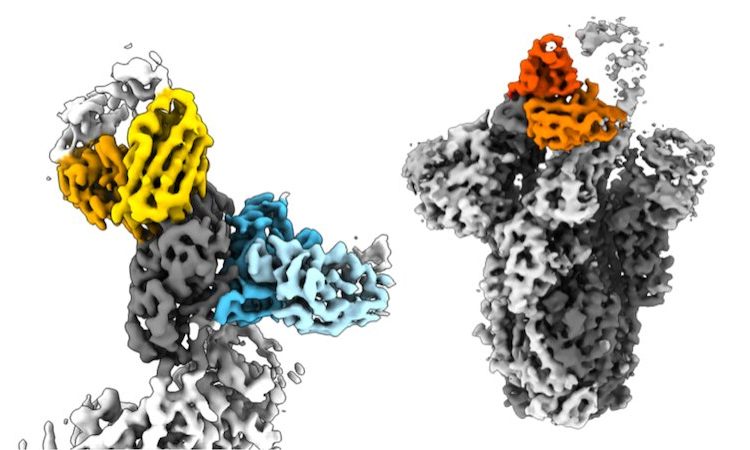
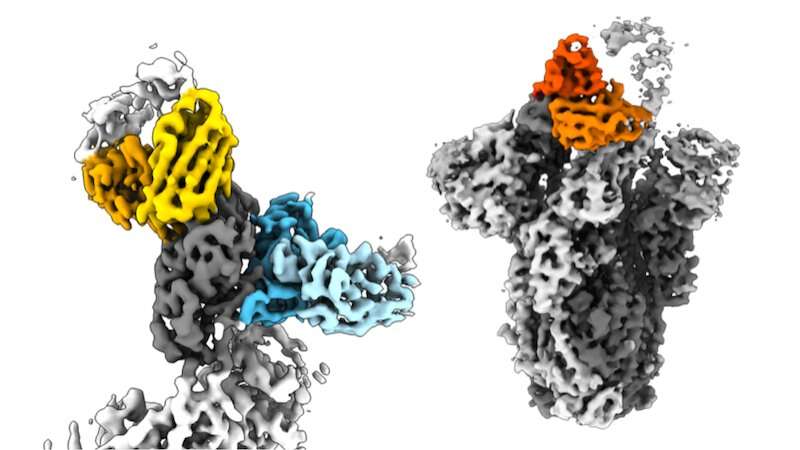
The scientists went on to map out these vulnerabilities on Spike using a high-resolution imaging technique called cryo-electron microscopy. “We were really interested to see how these antibodies recognize the Spike protein and structure,” says LJI Postdoctoral Fellow Xiaoying Yu, who co-led the new study with Hastie. “This structural work lets us see exactly how the antibodies interact with the protein and how they can neutralize the virus.”
The imaging work revealed that two of the promising antibodies bind to the SARS-CoV-2 Spike by latching onto two parts of the protein at once. By capturing Spike in a sort of hug of death, these antibodies lock the viral structure in place to halt infection. This finding is consistent with another recent Cell Reports study from the Saphire Lab showing the importance of bivalent antibodies against SARS-CoV-2 variants.
Could these three promising antibodies be recreated in an antibody therapeutic to treat COVID-19? The results from a mouse model are encouraging. The LJI team found that each antibody by itself could indeed reduce the viral load in the lungs in mice infected with SARS CoV-2 BA.1 and BA.2.
Going forward, the researchers plan to run more human antibodies through this same pipeline at LJI—from antibody isolation to screening, structural analysis, and animal model experiments. “We can carry out the entire pipeline of antibody discovery now,” says Yu. “This research will help us combat the variants we have right now and give us targets for future vaccine development and therapeutics.”
More information:
Kathryn M. Hastie et al, Potent Omicron-neutralizing antibodies isolated from a patient vaccinated 6 months before Omicron emergence, Cell Reports (2023). DOI: 10.1016/j.celrep.2023.112421
Journal information:
Cell Reports
Source: Read Full Article