Queen Mary University of London researchers have discovered a new immune mechanism in osteocytes, the most common type of bone cell, that could lead to new drugs for breast and prostate cancer.
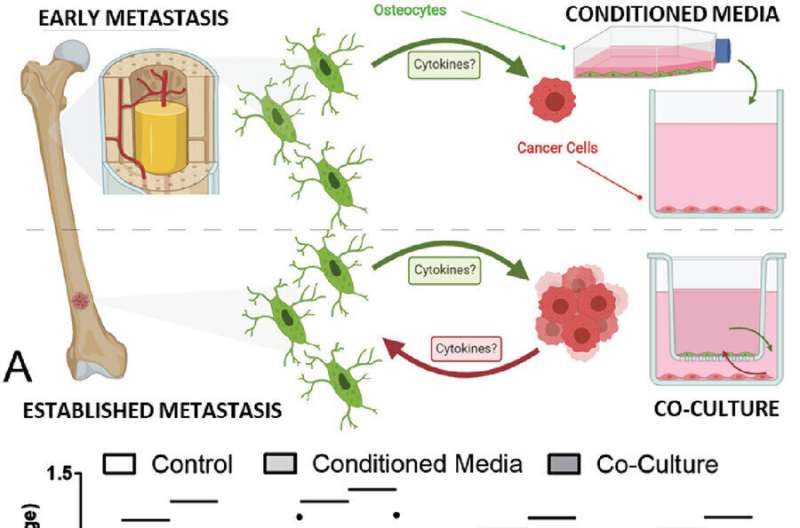
The study, published in Advanced Science, found that osteocytes can use this mechanism to suppress the growth of invading breast and prostate cancer cells. However, cancer cells can intervene to prevent bone cells from developing this feature, resulting in a promotion of tumor growth.
While survival rates in breast and prostate cancer—the two most common cancers—have increased thanks to improvements in screening and treatment, these patients have high levels of pain and lower survival chances if the cancers spread (metastasize) into their bones, a common progression.
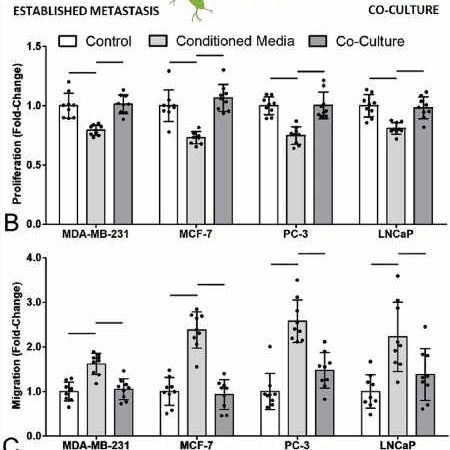
The interaction between bone cells and cancer cells has previously been poorly understood, so the study aimed to investigate how breast and prostate cancers spread to, and grow within bones. Using cell culture and organ-on-a-chip technology, it identified a new mechanism through which they hijack our bone cells in order to grow faster.
The study found that osteocytes, by far the most common bone cell type making up more than 90% of our bone cells, possess an immune mechanism that they can use to suppress the growth of invading breast or prostate cancer cells. However, a vicious feedback loop is created when the cancer cells intervene to prevent the bone cells from developing this feature and therefore block this suppression, resulting instead in a promotion of tumor growth.
It is probable that this initial inhibition of the cancer cells by osteocytes could in some part explain why breast and prostate cancers often go dormant before establishing metastatic colonies in bone tissue.
The discovery of this new molecular mechanism demonstrates the importance of cancer cell to osteocyte signaling in regulating breast and prostate bone metastases, and further supports the development of therapies which target and disrupt this pathway.
Most notably, these findings reveal two specific new drug targets which could be used to either support the osteocyte suppression of the cancer cells by TNF-α, or prevent the cancer cells from blocking this suppression via TGF-β.
Dr. Stefaan Verbruggen, Lecturer in Medical Technology in the School of Engineering and Materials Science at Queen Mary University says, “Most importantly and unusually, as this mechanism affects both breast and prostate cancer, the most common cancers, the number of patients who may benefit is massive.”
Continuing work with the bone metastasis organ-chip model will allow the team to develop a more complex 3D human tumor microenvironment and therefore further investigate and test these new identified therapies.
The work was part of a Marie Curie Fellowship for Stefaan Verbruggen and a collaboration between Professor Martin Knight at Queen Mary University of London and Professor Chris Jacobs at Columbia University, who sadly passed away from cancer before the study was completed. The paper contains a dedication to his memory.
More information:
Stefaan W. Verbruggen et al, A Novel Primary Cilium‐Mediated Mechanism Through which Osteocytes Regulate Metastatic Behavior of Both Breast and Prostate Cancer Cells, Advanced Science (2023). DOI: 10.1002/advs.202305842
Journal information:
Advanced Science
Source: Read Full Article