An international team of scientists, including those at the Translational Genomics Research Institute (TGen), an affiliate of City of Hope, has devised a tool that could help design more successful clinical trials for new brain-tumor drug treatments.
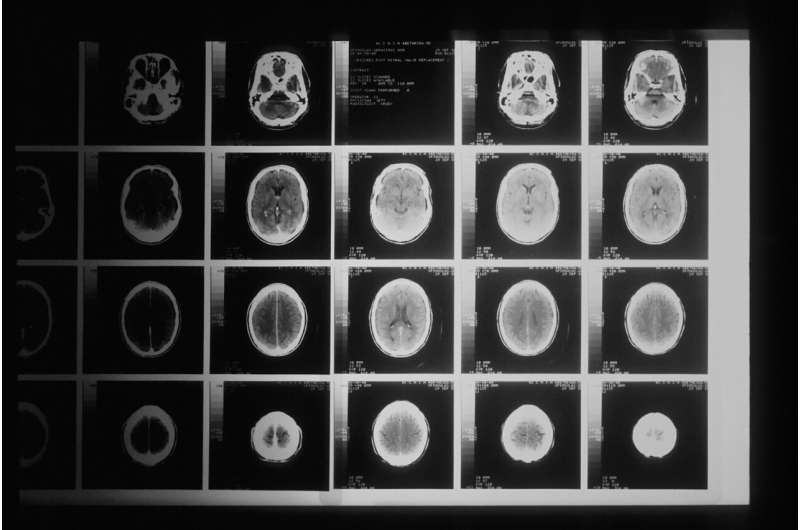
Findings from an international study published in the Journal of Neuro-Oncology suggest that a tool called a nomogram could help predict the likely survival time of individual patients with glioblastoma, the most common malignant brain cancer in adults, with an average survival of less than two years.
However, survival times vary among patients because of numerous factors, including age, where the tumor is located, how much of the tumor is removed through surgery, and—most importantly in this study—the patient’s sex.
It is now well established that males are more likely than females to develop glioblastomas, and that females respond to treatments at almost twice the rate of males. If these factors are not considered in selecting clinical trial participants, the results could be skewed because of an imbalance among those receiving a new treatment and those receiving the current standard-of-care. Faulty results could lead to the approval of a drug that has little or no value, or the rejection of a drug that actually could benefit particular patients.
“The more balanced the experimental and control treatment arms are, the higher the likelihood that researchers draw efficacy conclusions that stand up in routine clinical use,” said Michael Berens, Ph.D., Professor and Director of TGen’s Cancer and Cell Biology Division, and one of the study’s authors.
“If we miss some active drugs because we stacked the deck against ourselves, it would be tragic,” said Dr. Berens, who also is a TGen Deputy Director of Institutional Initiatives. “You must find subsets of patients with better chances of benefiting from a specific, new treatment. Get them the drug. That’s called precision medicine.”
Study based on more than 1,300 patients
In creating a nomogram for glioblastoma, the study examined the outcomes in two clinical trials among 1,359 patients newly-diagnosed with glioblastoma.
“The differences in the nomograms by sex shown here indicates that the prognosis of females and males may be different, and that these nomograms are useful tools for estimating patient-level survival probabilities,” the study concludes, recommending that additional research be conducted to better characterize the exact biological mechanisms underlying sex differences in glioblastoma.
Nomograms for other cancers are used in oncology and medicine to generate the probability of clinical events by integrating variables to produce biological and clinical models that help with treatment decisions.
“Nomograms for glioblastoma fill a significant unmet need in the design of clinical trials of new treatments for this deadly brain cancer, for which patients have few treatment options,” said Jill Barnholtz-Sloan, Ph.D., the study’s senior author, previously the Sally S. Morley Designated Professor for Brain Tumor Research at Case Western Reserve University School of Medicine, and Director for Research Health Analytics at University Hospitals of Cleveland (both in Cleveland, Ohio).
Source: Read Full Article
