New research hints at a possible explanation as to why people with diabetes, asthma and other conditions that involve chronic inflammation are more susceptible to the coronavirus and tend to experience more serious COVID-19.
The pre-print study—which is being submitted to a scientific journal but hasn’t yet undergone peer review by other researchers—found the virus that causes COVID-19 infected more cells in lab-made blood capillaries, or tiny blood vessels, that were treated with an inflammatory agent.
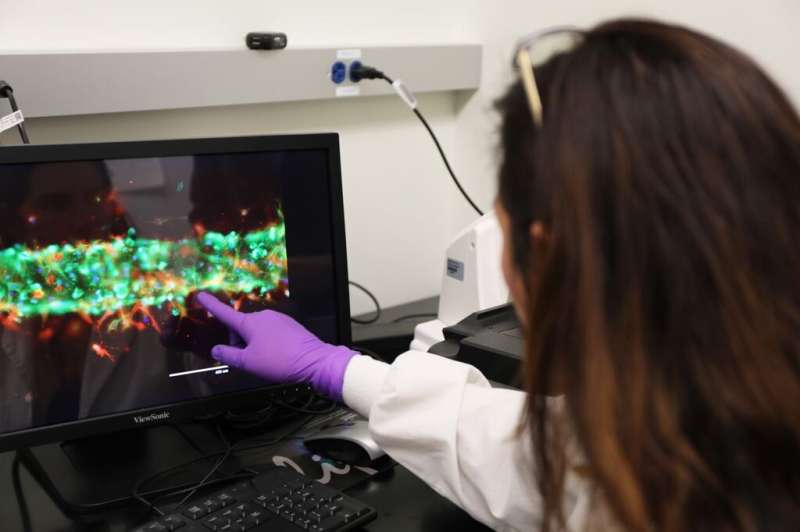
To conduct this study, Oregon Health & Science University researchers engineered blood capillaries in small, transparent devices etched with tiny channels. The scientists filled those channels with cultures of two types of cells: stem and endothelial. Endothelial cells line the interior of blood vessels and capillaries and are also involved in the body’s inflammatory response, while stem cells have the unique ability to develop into other cell types. Inside the transparent device, the stem cells naturally developed into pericyte cells, which wrap around endothelial and help manage blood flow in blood vessels and capillaries.
The researchers describe their setup as vasculature-on-a-chip, and were inspired by the research approach known as an organ-on-a-chip, which creates microscopic organ models for laboratory research. This study builds on previous research, which has indicated pericytes are involved in COVID-19 symptoms such as myocarditis, cognitive challenges and long COVID.
“This study adds another piece to the puzzle as we work to unravel COVID’s inner workings,” said the study’s senior author, Luiz Bertassoni, D.D.S., Ph.D., who is an associate professor of biomaterials and biomechanics in Oregon Health & Science University’s School of Dentistry, as well as an associate professor of biomedical engineering in the OHSU School of Medicine and the OHSU Knight Cancer Institute.
The study’s first author, Cristiane Miranda França, D.D.S., M.S., Ph.D., a research assistant professor of restorative dentistry in the OHSU School of Dentistry, and colleagues created two models to simulate large and small blood capillaries. Copies of each model size were either treated with a pro-inflammatory chemical known as TNF-alpha to recreate inflamed capillaries, or went without this treatment to recreate healthy capillaries. The researchers exposed the lab-made capillaries to spike proteins from the virus that causes COVID-19, and then compared the tissues under a microscope.
They found significantly more spike proteins attached to the lab-made capillaries that were treated with the inflammatory agent. The authors hypothesized that chronic inflammatory health conditions, such as obesity, diabetes and asthma, could be particularly dangerous to pericytes. The researchers suggest this could, in turn, make it easier for SARS-CoV-2 to pass through vessels, proliferate and spread throughout the body.
“Inflammation appears to expose pericytes more to SARS-CoV-2, the virus that causes COVID-19,” Bertassoni said. “Better understanding [of] the vascular mechanisms behind this could help us find new ways to treat or prevent COVID.”
Source: Read Full Article
