Reviewers’ Notes
OCT-guided PCI does not reduce target vessel failure in complex patients, but improves safety
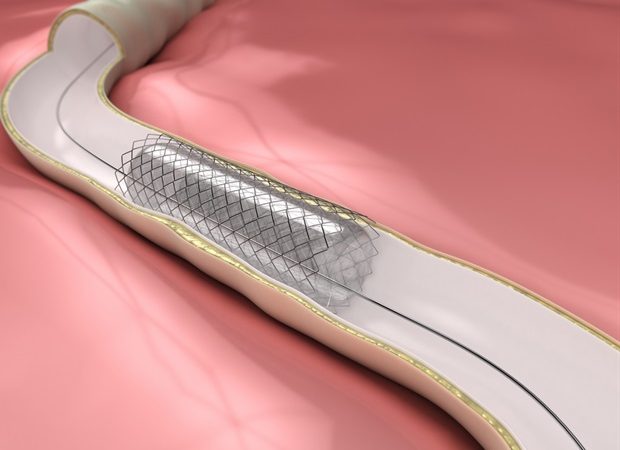
Optical coherence tomography (OCT)-guided percutaneous coronary intervention (PCI) leads to a larger minimum stent area but does not reduce the two-year rate of target vessel failure compared with angiography-guided PCI, according to late breaking research presented in a Hot Line session today at ESC Congress 2023. Stent thrombosis was significantly reduced with OCT-guided PCI.
Previous randomized trials have demonstrated improved clinical outcomes with intravascular imaging-guided PCI compared with angiography guidance alone, including in complex patients. These findings have led to a Class IIa recommendation in ESC Guidelines. The ILUMIEN IV trial investigated whether OCT-guided PCI is superior to angiography-guided PCI for minimum stent area and target vessel failure in complex patients and lesions.
The trial enrolled patients with medication-treated diabetes and/or complex lesions (defined as non-ST-segment elevation myocardial infarction [NSTEMI], late-presenting ST-segment elevation myocardial infarction [STEMI; >24 hours], stent length ≥28 mm, severe calcification, two-stent bifurcation, in-stent restenosis or chronic total occlusion) at 80 sites in 18 countries. The investigators chose to include only complex patients and complex lesions as these patients were considered the most likely to gain the benefit of OCT guidance. Patients were randomized in a 1:1 ratio to OCT-guided PCI or angiography-guided PCI. Blinded OCT was performed after PCI in the angiography group to enable assessment of the first co-primary endpoint and other differences between the two treatment arms. Patients and post-procedure research personnel were blinded to treatment assignment.
The co-primary endpoints were 1) the post-PCI minimum stent area (an independent predictor of future adverse events after drug-eluting stent implantation) assessed by OCT and 2) the two-year rate of target vessel failure, defined as a composite of cardiac death, target vessel myocardial infarction or ischemia-driven target vessel revascularization. Safety was also assessed.
The trial included 2,487 patients, of whom 1,233 received OCT-guided PCI and 1,254 received angiography-guided PCI. The mean age of participants was 65.6 years and 22.6% were women. For efficacy, the minimum stent area achieved was larger in the OCT-guided group than in the angiography-guided group (5.72 ± 2.04 vs. 5.36 ± 1.87 mm2; difference 0.36 mm2, 95% confidence interval [CI] 0.21 to 0.51; p<0.001). Target vessel failure within two years occurred in 88 OCT-guided patients and 99 angiography-guided patients (Kaplan-Meier estimated rates 7.4% vs. 8.2% respectively; hazard ratio [HR] 0.90; 95% CI 0.67 to 1.19; p=0.45).
Regarding safety, there were fewer angiographic complications with the OCT guidance strategy. In addition to the larger minimum stent area, OCT guidance resulted in fewer cases of major dissection, malapposition, tissue protrusion and untreated reference segment disease. Stent thrombosis within two years occurred in 6 (0.5%) OCT-guided patients and in 17 (1.4%) angiography-guided patients (HR, 0.36; 95% CI, 0.14 to 0.91). The number of cardiac deaths and myocardial infarctions were fewer in the OCT arm, although these differences were not statistically significant.
OCT-guided PCI led to a larger minimum stent area, enhanced the safety of the PCI procedure and resulted in a nearly two-thirds reduction in stent thrombosis during two-year follow-up. However, in this trial OCT guidance did not reduce the two-year rate of target vessel failure compared with angiography-guided PCI because of a low and nearly identical rate of target vessel revascularization in the OCT-guided and angiography-guided PCI arms."
Dr. Ziad Ali, Study Author, St. Francis Hospital, Roslyn, US
European Society of Cardiology (ESC)
Posted in: Medical Procedure News | Medical Research News | Medical Condition News
Tags: Angiography, Calcification, Cardiology, Chronic, Diabetes, Drug-Eluting Stent, Efficacy, Hospital, Imaging, Myocardial Infarction, OCT, Optical Coherence Tomography, Research, Restenosis, Stent, Thrombosis, Tomography