In an advance that sheds light on why certain vaccines may influence people differently, a new computational approach developed at the University of Michigan may predict how individual patients are likely to respond.
In the future, it could lead to new design principles for vaccines that take an individual’s personalized characteristics into account, possibly enabling vaccines for HIV and more effective protection from the flu.
“Different people vary in the amount and type of antibodies they produce,” said Kelly Arnold, a U-M assistant professor of biomedical engineering and a corresponding author on a new study published in Cell Reports Medicine. “Depending on their genetics, they also have different protein sequences in their antibodies and immune cell receptors that cause them to bind differently.
“That situation is difficult for researchers to understand based on experiments. And that’s why this computational model has been so valuable. We can make personalized models for different people that take all of these different factors into account.”
Vaccines can work in two ways: by sending neutralizing antibodies to bind an invasive virus and prevent it from infecting cells, or by activating innate immune cells to attack pathogens. The former works for relatively static viruses, like measles, but for viruses like HIV and flu, activating immune cells can make up for the fact that antibodies aren’t always a perfect match for the virus. The trouble is that the type and amount of the antibodies can influence immune cell activation differently, as shown by the study, published in Cell Reports Medicine.
“With rapidly mutating viruses like HIV and the flu, there is variability in both the viral population and the people it’s infecting,” said Melissa Lemke, a U-M Ph.D. candidate in biomedical engineering and lead author on the paper. “This means that in order to protect all people to the same degree from a variety of viral mutations, we will need an array of possible solutions that can be matched to any given person’s health status, sex, age, and genetic background.”
“Computational tools like this one are going to be essential in speeding up the search for mechanisms that can be implemented to create effective vaccines for all.”
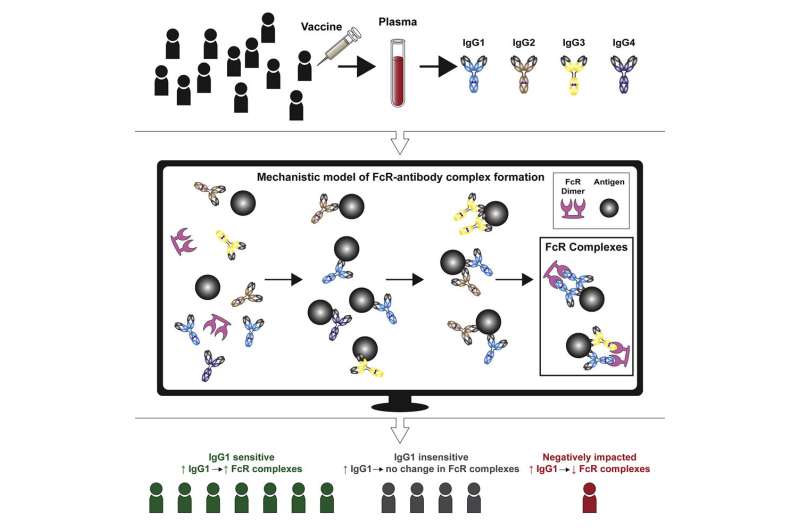
The U-M model used data obtained by the University of Melbourne from the only moderately protective HIV vaccine trial to date. The model examined plasma samples from trial participants—basically blood samples minus the red blood cells—looking at the amount and type of antibodies produced after vaccination. When an antibody binds to a pathogen and to an immune cell, this is the signal for the immune cell to destroy the pathogen.
The model predicted that boosting levels of antibodies does not activate immune cells across the board for all individuals. Depending on a subject’s baseline antibody levels and genetic background, increasing those antibodies can produce results running the gamut from benefiting some patients, to doing nothing for others, to potentially reducing immune cell activation in others.
The U-M team evaluated 30 people from the trial and selected the eight whose immune cell receptors were most likely to bind with vaccine-induced antibodies, and the eight least likely to respond well. Then, the team at Melbourne ran experiments adding antibodies and HIV viruses to plasma samples. Those predicted to respond saw a 5-7-fold increase in immune complexes—made up of an antibody, pathogen and immune cell—that indicate virus-killing activity. In contrast, non-responders saw only a 1.3-fold increase in immune complexes. This shows that making antibodies that bind well to the virus is not necessarily enough to make a vaccine protective—the immune cells need to be able to bind to the antibodies.
Source: Read Full Article
