Using demographic information, brain imaging test results and genetic biomarkers, researchers at Washington University School of Medicine in St. Louis have developed an algorithm that can help provide people who volunteer for studies of aging with information about the risk each faces of developing dementia due to Alzheimer’s disease.
Published Sept. 30 in the Alzheimer’s & Dementia journal, the findings—from researchers with the university’s Knight Alzheimer Disease Research Center (Knight ADRC)—may help study participants learn more about what their futures hold, in terms of risk for dementia related to Alzheimer’s. The research also eventually may help others determine whether they face risk of the debilitating disorder.
“Thousands of adults have volunteered for studies at Alzheimer’s research centers around the country,” said principal investigator Sarah M. Hartz, MD, Ph.D., an associate professor of psychiatry.
“They come back and undergo tests year after year, including PET (positron emission tomography) and MRI scans, blood draws, cognitive tests, and lumbar punctures that measure proteins in spinal fluid. Those studies advance the overall understanding of Alzheimer’s disease, but they give participants relatively little information about their own risk. This algorithm is a way to help illuminate that information and to let individuals know whether they have a significant risk for dementia related to Alzheimer’s disease.”
Hartz and co-principal investigator Jessica Mozersky, Ph.D., an assistant professor of medicine in the university’s Bioethics Research Center, examined the various factors that contribute to Alzheimer’s dementia, and they used that information to create an algorithm aimed at estimating an individual’s absolute risk of developing early symptoms of dementia from Alzheimer’s. They developed the algorithm for use in a clinical trial to learn whether they could help volunteers participating in aging studies at the Knight ADRC better understand what biomarkers for disease they might have, and whether researchers then could evaluate participants’ eventual outcomes.
“We developed the algorithm because study participants wanted more than just a report of whether their test results were normal or abnormal,” Mozersky said. “We’ve performed studies with people who receive results reporting elevated amyloid, for example. They tell us, “You know what I really want to know? My risk.'”
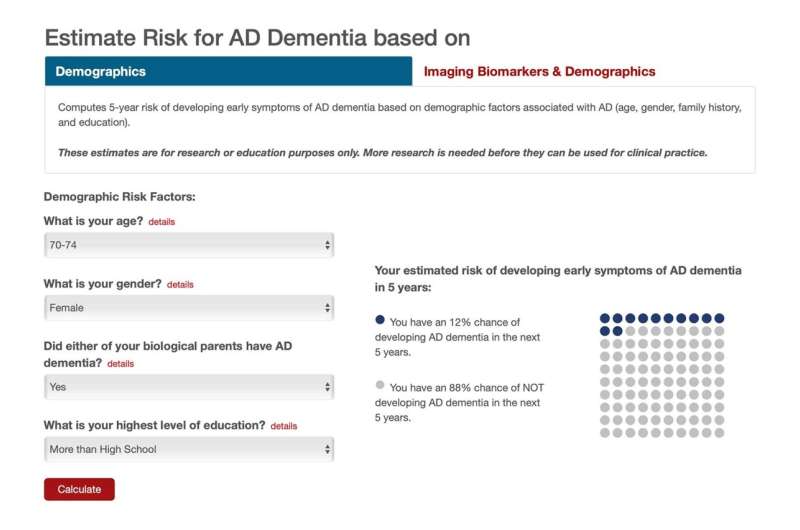
The website with the risk algorithm uses demographic information, along with specific test results, to help study volunteers better understand their risk.
Over the years, there have been ethical debates about how much information to release to people who participate in such studies because there aren’t yet any treatments to prevent or cure Alzheimer’s dementia. Further, how well various biomarkers predict the problem in people who have no symptoms of the disorder has not been well studied.
“We developed the algorithm so that we can tell participants what currently is known in a meaningful way, and so that the algorithm can be updated easily as new research or data emerges,” Hartz said.
The algorithm, accessible on the Knight ADRC’s website, provides greater detail for researchers and individuals who want to learn more about Alzheimer’s dementia risk. For example, a 69-year-old woman who went to college and had a parent with dementia from Alzheimer’s has about a 6% risk of developing the early symptoms of Alzheimer’s dementia in the next five years. That, of course, means she also has a 94% chance of not developing dementia from Alzheimer’s in the next five years.
The algorithm incorporates amyloid PET scan results and brain hippocampal volumes—a smaller hippocampus often suggests an increased risk for damage related to Alzheimer’s dementia—to show how risk changes when such extra information is known. If that same 69-year-old woman also had a PET scan revealing elevated levels of amyloid, and a decrease in hippocampal volume, her risk would rise to about 33%.
“Still, age is the biggest demographic risk factor,” Hartz said.
If the woman was 85 years old rather than 69, her risk of developing dementia from Alzheimer’s in the next five years would climb from about 6% to about 32%, even without knowing any biomarker-related results.
The researchers also looked at a gene known to influence risk of Alzheimer’s dementia. Risk increases significantly depending on the type of APOE gene a person has. But when the researchers included APOE genotype in their model, they found it didn’t tell them anything that data from imaging tests hadn’t already revealed. This is likely because brain changes seen on imaging tests occur in part because of the APOE gene.
Hartz and Mozersky are continuing their work to improve the ability to predict Alzheimer’s dementia risk based on these variables. They have grants totaling more than $5 million from the National Institute on Aging to run a clinical trial to better understand the impact of providing these risk assessments to people participating in research and to validate their algorithm in larger samples.
Source: Read Full Article
