Scientists at Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine, collaborating with international researchers, have developed a sophisticated AI algorithm that performs advanced computational analysis to identify potential therapeutic targets for glioblastoma multiforme (GBM) and other cancers.
Their research is described in the Feb. 2 issue of the journal Nature Cancer and could have profound implications for future treatment of GBM, an aggressive, usually fatal type of brain cancer, and certain breast, lung and pediatric cancers.
“Our work represents translational science that offers immediate opportunities to change the way glioblastoma patients are routinely managed in the clinic,” explained Antonio Iavarone, M.D., deputy director of Sylvester Comprehensive Cancer Center and senior author of the study. “Our algorithm offers applications to precision cancer medicine, giving oncologists a new tool to battle this deadly disease and other cancers as well.”
The AI algorithm, known as SPHINKS—Substrate PHosphosite-based Inference for Network of KinaseS—deployed deep-machine learning to help the researchers identify and experimentally validate two protein kinases (PKCδ and DNAPKcs) as the culprits associated with tumor progression in two GBM subtypes and as potential therapeutic targets for other cancers.
Protein kinases are the key targets currently used in precision cancer medicine to tailor treatment to a patient’s specific cancer properties. The most active kinases, which the researchers labeled “master kinases” in their paper, are those for which clinicians direct targeted drugs as a hallmark of current cancer treatment.
In addition to identifying the master kinases, Dr. Iavarone and colleagues used tumor organoids grown in the laboratory from patient samples—what they called “patient-derived tumor avatars”—to show that targeted drugs that interfere with the activity of master kinases can thwart tumor growth.
Previously, Dr. Iavarone and team had reported a new glioblastoma classification by capturing key tumor cell traits and grouping GBM patients based on their likelihood of survival and their tumor’s vulnerability to drugs. In the new study, these classifications were independently confirmed through several omics platforms: genomics (genes), proteomics (proteins) lipidomics (fat molecules), acetylomics (epigenetics), metabolomics (metabolites) and others.
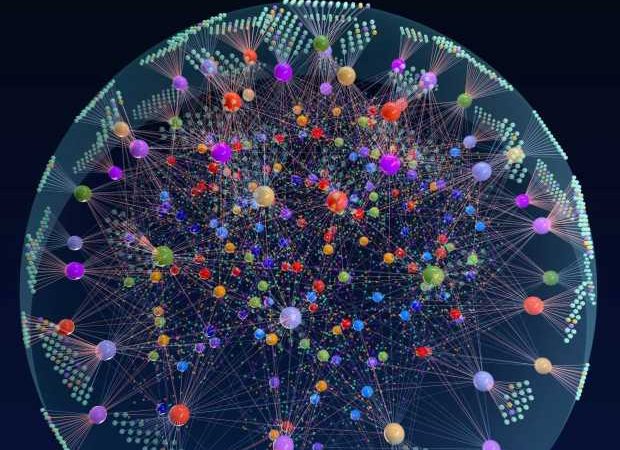
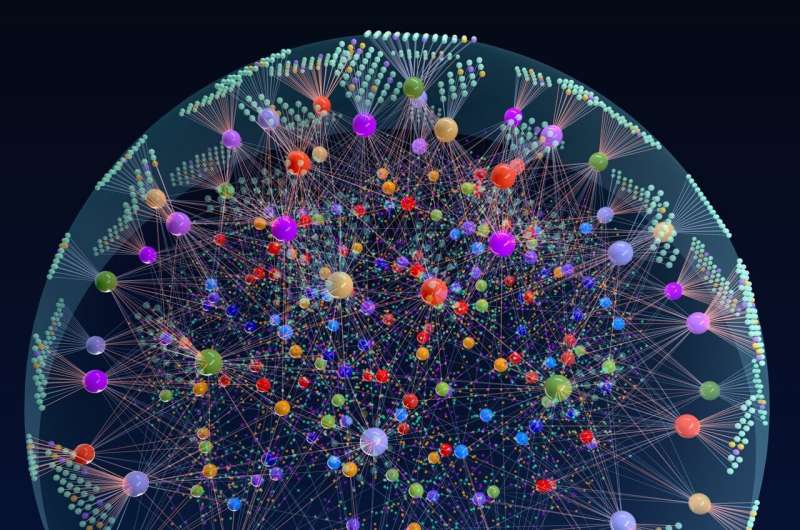
SPHINKS leverages machine learning to refine these omics datasets and create an interactome –a complete set of biological interactions—to pinpoint the kinases that generate aberrant growth and treatment resistance in each glioblastoma subtype. These findings show multi-omics data can generate new algorithms that predict which targeted therapies can provide the best therapeutic options based on each patient’s glioblastoma subtype.
“We can now stratify glioblastoma patients based on biological features that are common between different omics,” Dr. Iavarone said. “Reading the genome alone has not been enough. We have needed more comprehensive data to identify tumor vulnerabilities.”
Despite breakthroughs for many other cancers, glioblastoma patients face dismal prognoses—the five-year survival rate is below 10%. Although numerous drugs are being developed as potential therapy, clinicians have needed a way to identify the molecular mechanisms that drive each patient’s disease and are applicable to precision cancer medicine.
The SPHINKS algorithm and related methods can be readily incorporated into molecular pathology labs, according to the researchers. Their paper includes a clinical classifier that can help assign the appropriate glioblastoma subtype to each patient. The team has also established an online portal to access the algorithm. The authors believe this approach can produce insightful information that could benefit as many as 75% of glioblastoma patients.
“This classifier can be used in basically any lab,” said Anna Lasorella, M.D., professor of biochemistry and molecular biology at Sylvester CCC and co-senior author on the study. “By importing the omics information into the web portal, pathologists receive classification information for one tumor, ten tumors, however many they import. These classifications can be applied immediately to patient care.”
While SPHINKS was first tested on glioblastoma, the algorithm is equally applicable to several other cancers. The team found the same cancer-driving kinases in breast, lung and pediatric brain tumors. Drs. Iavarone and Lasorella and colleagues believe this finding could be the impetus for a new type of clinical trial.
“We are exploring the concept of basket trials,” Dr. Iavarone explained, “which would include patients with the same biological subtype but not necessarily the same cancer types. If patients with glioblastoma or breast or lung cancer have similar molecular features, they could be included in the same trial,” he continued. “Rather than doing multiple trials for a single agent, we could conduct one combined trial and potentially bring more effective drugs to more patients faster.”
More information:
Anna Lasorella, Integrative multi-omics networks identify PKCδ and DNA-PK as master kinases of glioblastoma subtypes and guide targeted cancer therapy, Nature Cancer (2023). DOI: 10.1038/s43018-022-00510-x. www.nature.com/articles/s43018-022-00510-x
Journal information:
Nature Cancer
Source: Read Full Article