Before we get vaccinated, most of us tend to ask: Will it hurt? Will I get a fever? Will the injection site be painful afterwards? But the question of whether repeat vaccinations are best given in the same arm, or first in the right arm and then in the left (or the other way round) is probably not a question anyone has asked up until now. That this question is significant is thanks to the work of a young research scientist at Saarland University in Germany.
“The question seems so banal, so trivial that nobody before has thought to ask it,” says Professor Martina Sester at the start of our conversation about the work of her doctoral student Laura Ziegler. What might at first sound like a bit of a put down is anything but—and it soon becomes clear that Sester values the fact that her doctoral student took the time to address this easily overlooked question.
Scientists like Martina Sester, Professor of Transplant and Infection Immunology at Saarland University, and Laura Ziegler, who are interested in examining the effectiveness of vaccinations and vaccines, are far more likely to ask questions like: How does the vaccine move through the body? Does it travel directly or indirectly to the target site, and does it do any damage to normal body cells on the way? Is this vaccine more effective than that one, and which has the longer immune response?
But so far no one has addressed the simple question of whether it’s better for a doctor to give sequential vaccination shots in the same arm or to deliver one in the left arm and one in the right.
That may now be about to change. “Our study indicates that ipsilateral vaccinations generate a stronger immune response than contralateral vaccinations,” explains Laura Ziegler. In an ipsilateral vaccination the vaccine is injected twice into the same arm. In a contralateral vaccination, the primary vaccination is delivered to the left arm while the booster is injected into the right arm, or vice versa. Germany’s COVID-19 vaccination campaign provided an ideal setting in which to study this question. Laura Ziegler and Martina Sester were able to create a reliable dataset of 303 individuals who received the mRNA vaccine from Biontech as their primary and booster shots at the start of Germany’s COVID-19 vaccination campaign.
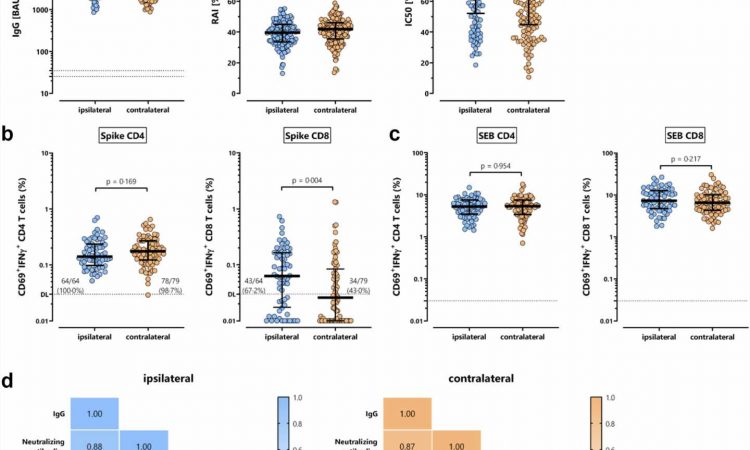
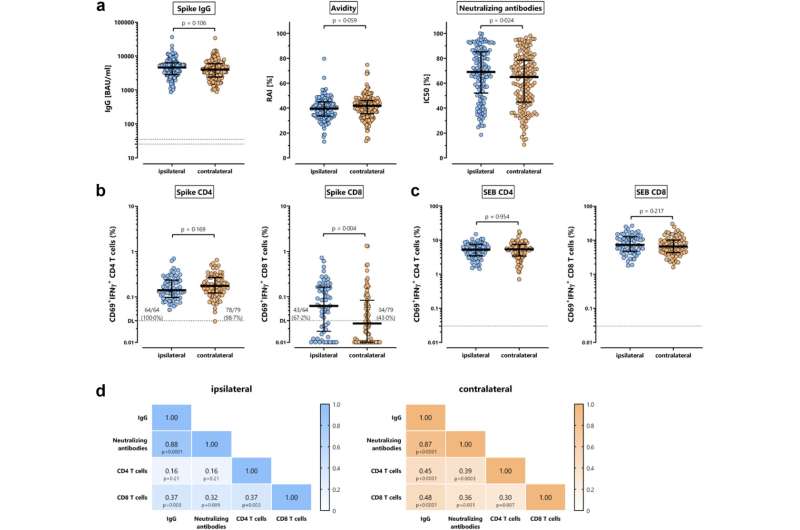
The most striking result was that two weeks after the booster shot the number of cytotoxic CD8+ T cells, often referred to as ‘killer T cells,’ was significantly higher in those individuals who had been injected in the same arm. “In the ipsilateral subjects, we were able to detect the killer T cells in 67 percent of cases. In contrast, we detected CD8+ T cells in only 43 percent of the contralaterally vaccinated subjects,” explains Laura Ziegler. That may suggest that that ipsilateral vaccination is more likely to provide better protection should the vaccinated person become infected with the SARS-CoV-2 virus.
“The number of antibodies, however, was not greater,” says Martina Sester. Unlike the killer cells, the antibodies do not immediately destroy the virus. Instead, they dock onto the virus preventing it from causing further harm or making it easier for macrophages to find the virus and then engulf and degrade it.
“What’s interesting is that the antibodies in the ipsilaterally vaccinated subjects were better at binding to the viral spike protein,” explains Sester. So the antibodies in those persons who were vaccinated in the same arm were better at doing their job than the antibodies in the contralateral subjects, who were given injections in both arms.
So far there have been hardly any studies looking into the significance of where primary and booster vaccination shots are applied. “As dramatic as the pandemic was, it has provided us with reliable data that enables us to address questions of this kind,” explains Professor Sester.
At the early stage of the vaccination campaign, there were a very large number of volunteers who had not had any contact with the SARS-CoV-2 virus. Had their immune systems already been in contact with the pathogen, this would have affected the results of the study.
As it was, all 303 immune systems had identical starting conditions with respect to COVID-19. For medical scientists like Laura Ziegler and her supervisor Professor Martina Sester, the pandemic provided a unique opportunity to examine questions about immune response mechanisms.
As Laura Ziegler only analyzed data from individuals who had received two shots of the Biontech SARS-CoV-2 vaccine, the 23-year-old researcher is suitably cautious about generalizing the conclusions of her study. Further work is required before we know whether the study has implications for other sequential vaccinations, such as flu vaccinations or vaccinations against tropical diseases.
But it does seem possible that some vaccinations will generate a stronger immune response if the injections are delivered into the same arm—making the apparently naive question posed at the beginning of the study suddenly seem not quite so banal after all.
The paper is published in the journal eBioMedicine.
More information:
Laura Ziegler et al, Differences in SARS-CoV-2 specific humoral and cellular immune responses after contralateral and ipsilateral COVID-19 vaccination, eBioMedicine (2023). DOI: 10.1016/j.ebiom.2023.104743
Journal information:
EBioMedicine
,
JCI Insight
Source: Read Full Article