Using data from over 300 patient tumors, UCSF researchers have described 12 classes of “immune archetypes” to classify cancer tumors. Their findings, published this week in Cell, reveal that cancers from different parts of the body are immunologically similar to one another. These classifications provide unique strategies for enhancing each patient’s choice of cancer immunotherapies.
The UCSF researchers, led by first co-authors Alexis Combes, Ph.D., and Bushra Samad, MS, and senior author, Max Krummel, Ph.D., obtained tumor specimens from 78 UCSF clinicians, and surveyed 364 tumors biopsies from patients and categorized them into groups based on their immune microenvironment. Their findings offer a new way of looking at cancer immunotherapy that matches the immune environment around the tumor and points the way to personalized immunotherapies.
“This is a new framework for how to look at cancer patients,” said Combes, director of the D2B CoLab and incoming assistant professor in the Department of pathology at UCSF. “This work will help clinicians find the right biology to target and avoid targeting cells that aren’t present in the tumor.”
Immunotherapy for cancer treatment harnesses the body’s immune system to fight cancer. It has held great promise since it was first developed as a biological therapy used to treat a variety of cancers. While it has proven successful for some patients, immunotherapy does not work for all patients.
“We were driven by this question of why immunotherapies work for some people and not others,” said Krummel, Robert E. Smith Endowed Chair in Experimental Pathology and director of the Krummel Lab at UCSF. “It’s more complex than responders and non-responders. Our goal was to discern how many responses there are to these targeted therapies.”
Tumors have microenvironments
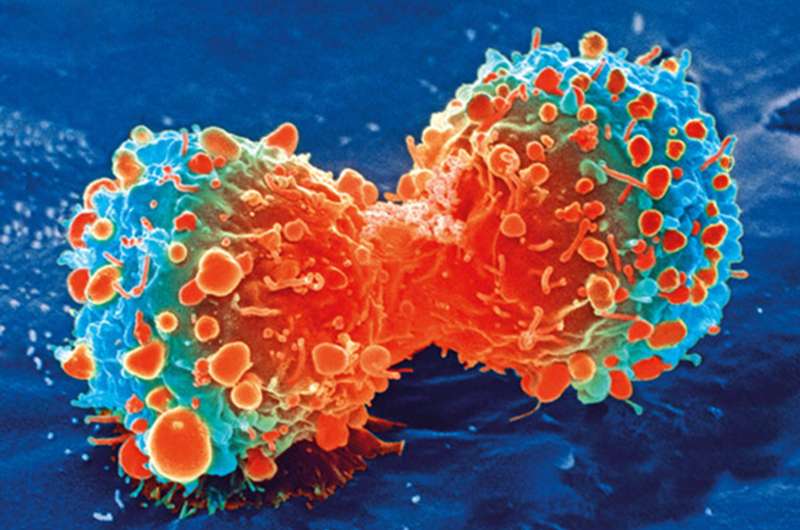
Tumors are more than just out-of-control cells. They are also filled with immune cells which are supposed to kill the cancer cells. But in cancer, malignant cells are able to overcome the body’s immune response and continue to multiply.
The research team found that a variety of cancers come in prescribed forms, each of which represents a unique subversion of the body’s immune defenses. The researchers characterized different microenvironments in the tumors, looking at which immune cells were present and which genes were expressed.
“We could see that the tumors and their environments inform each other,” said Combes.
The research team was able to group the tumors into 12 groups, which they call archetypes. To their surprise, the tumors contained a wide range of immune cells, such as macrophages, NK and B cells—beyond the T cells which are the focus of current immunotherapies.
Their research indicates that the immune archetype of a tumor is not necessarily tied to a type of cancer. Some archetypes are largely drawn from just a few kinds of cancer. Others draw from many. This means that some melanomas are quite similar to some lung tumors but more biologically different than other melanomas.
“Unbiased interrogation of multiple data sources including genetic sequencing, cell surface markers, imaging, and patient clinical data, set the groundwork atop which we were able to identify and describe these immune archetypes,” said Samad.
Identifying patients for clinical trials
The classification scheme not only identifies which tumors are likely to be vulnerable to current immunotherapies, it also helps identify which patients might be most responsive in which clinical trial.
“This framework allows us to eliminate a bunch of noise,” said Krummel. “We may have been targeting cells that weren’t even in the tumor.”
Clinicians and researchers contribute knowledge
Krummel’s research team was able to bring together a large group of UCSF researchers and clinicians—78 in all—who lent expertise across disciplines. The authors came together with the common goal of better leveraging promising therapies. This dual viewpoint and large body of knowledge is an approach being fostered by UCSF’s CoLabs.
Source: Read Full Article
