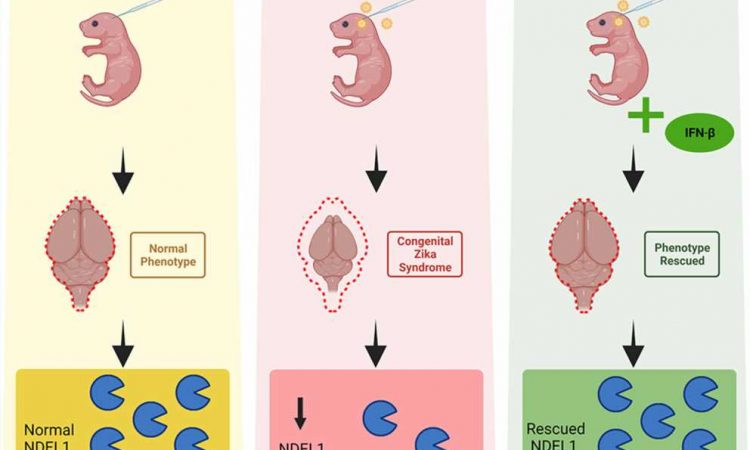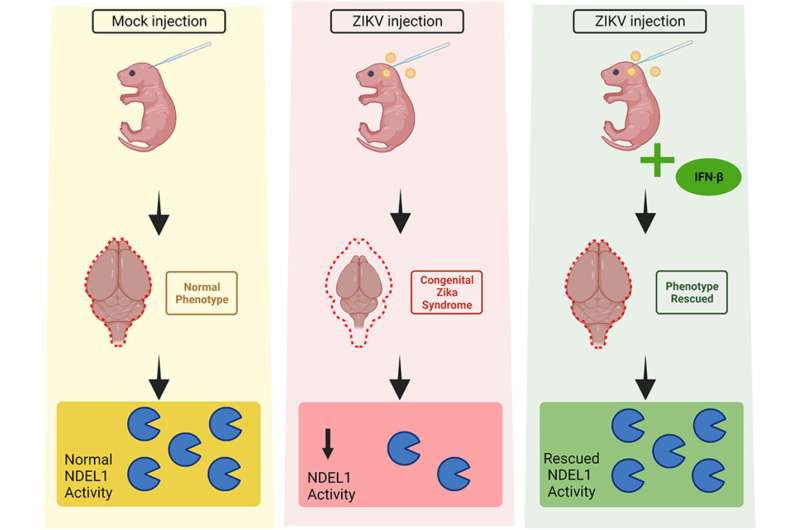
Mice that were infected with Zika virus during pregnancy and developed microcephaly displayed less activity of Ndel1, an enzyme that plays a key role in neuron proliferation, differentiation and migration during embryo development, according to an article published in the Journal of Neurochemistry.
The discovery has been patented and could serve in future as a basis for the development of a biomarker for early diagnosis of microcephaly in human babies infected with Zika during the embryonic period.
“We lack good biomarkers for early diagnosis [in the embryonic stage] of the congenital syndrome associated with infection by Zika. The discovery of this link between Ndel1 activity and brain size is only the beginning of the journey but offers great hope. Diagnosis is currently limited to measuring brain size by ultrasound or tomography, or based on imprecise measurement of the baby’s skull circumference after birth when little can be done to reverse the condition,” said Mirian Hayashi, last author of the article and a professor in the Department of Pharmacology at the Federal University of São Paulo’s Medical School (EPM-UNIFESP) in Brazil.
The researchers also observed positive effects of treatment with interferon-beta, a drug that is generally prescribed for multiple sclerosis and has been tested on animals infected by Zika. In experiments involving mice, interferon-beta avoided neuronal development problems and restored Ndel1 activity to levels similar to those seen in mice not infected by Zika.
Experimental model
The experimental model built by scientists at UFRJ enabled the authors to analyze Ndel1 activity and the action of interferon-beta in animals infected by Zika at different stages of embryo development in order to determine the risk of neurodevelopmental disturbances.
“We observed an association between the infection and reduced Ndel1 activity in the brain. We varied the conditions, injecting the virus into the ventricle of the embryo in the womb, for example, and we also varied viral load and the stage of embryo development. All this suggested that Ndel1 activity has outstanding diagnostic potential,” said João Nani, second author of the article. He is a Ph.D. candidate at UNIFESP.
Low Ndel1 activity does not necessarily mean the enzyme is less expressed or contains less protein. “In the article, we suggest its activity may be associated with either of two factors: the breakdown of chemical substances produced by brain cells [cleaving of neuropeptides, to be confirmed by future in vivo studies] or the enzyme’s capacity to interact with other proteins. Ndel1 interacts with many key proteins, and a reduction in its activity may alter important molecular dynamics,” Nani said.
Maternal-fetal infection
As Hayashi explained, infection by Zika during pregnancy can cause a series of malformations in offspring, including microcephaly, but many disorders can culminate in microcephaly or other kinds of brain damage during pregnancy, such as toxoplasmosis, measles, cytomegalovirus and herpes simplex, for example.
“Why did we decide to investigate this enzyme in cases of infection by Zika? Because it’s an excellent model for maternal-fetal infections in general,” she said. “We know the infection tends to trigger several responses, and in pregnancy this can mean complications for embryogenesis.”
Interest in Ndel1 among scientists has steadily increased owing to its importance to neurological development and disorders such as schizophrenia and depression. Furthermore, Hayashi noted, it is associated with the formation of complexes in the intracellular neuronal cytoskeleton, as well as neuron proliferation, differentiation and migration—and hence brain development—during embryogenesis.
The cytoskeleton proteins with which Ndel1 interacts include LIS1, which can cause defective neural migration leading to lissencephaly, or smooth brain, characterized by thickened cortical gray matter layer lacking the normal folds (gyri) in newborns. Ndel1 is also the major ligand for DISC-1, the most widely studied schizophrenia susceptibility gene.
Mutations in the gene NDE1 (which encodes a protein similar to Ndel1, called NDE1) have been associated with severe microcephaly in previous research. Experiments with animal models showed that inactivation of NDE1 or Ndel1 inhibits neuron migration in early embryo development.
“Our work has also shown that Ndel1 activity is significantly reduced in individuals experiencing a first psychotic episode without prior treatment with anti-psychotics and in chronic schizophrenia patients, suggesting that Ndel1 activity is a potential biomarker for initial stages of schizophrenia and resistance to treatment, although this has yet to be confirmed,” Hayashi said.
More information:
Raissa R. Christoff et al, Assessing the role of Ndel1 oligopeptidase activity in congenital Zika syndrome: Potential predictor of congenital syndrome endophenotype and treatment response, Journal of Neurochemistry (2023). DOI: 10.1111/jnc.15918
Journal information:
Journal of Neurochemistry
Source: Read Full Article