New research presented this week at ACR Convergence 2022, the American College of Rheumatology’s annual meeting, showed that discontinuing methotrexate for one week after seasonal influenza vaccination provided the same seroprotection as a two-week discontinuation period in patients with rheumatoid arthritis.
Methotrexate (MTX) remains a first-line therapy for rheumatoid arthritis (RA) due to its efficacy, favorable safety profile and cost. Yet it significantly reduces response to pneumococcal and seasonal influenza vaccines, especially novel strain antigens. Previous research showed that withholding MTX for two weeks after patients received the seasonal flu vaccine improved immunogenicity. This study aimed to determine whether a one-week hold of MTX was equally effective in terms of immediate and long-term vaccine response.
Jin Kyun Park, MD, Chief of Rheumatology at Seoul National University Hospital, associate professor at Seoul National University College of Medicine, and the study’s lead author, says the main reason for undertaking the trial was to determine whether the time without MTX could be minimized to reduce the likelihood of disease flares.
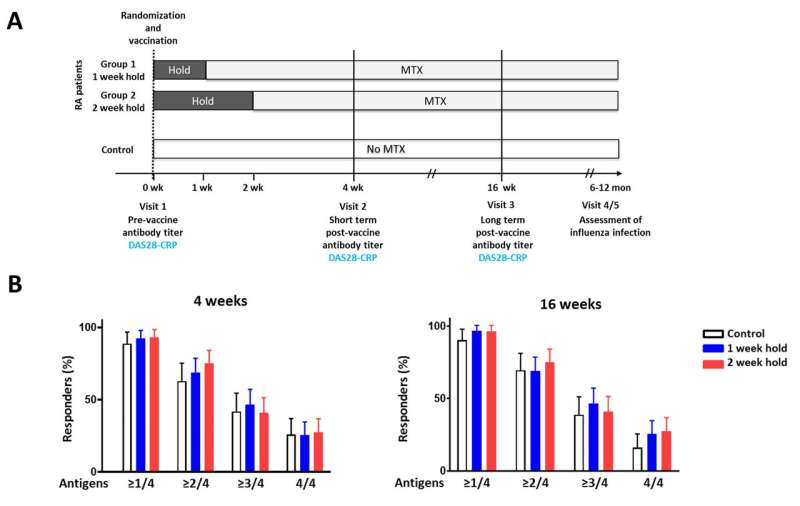
For this prospective randomized parallel-group trial, 178 adult patients with RA were recruited from tertiary centers in South Korea. All met the American College of Rheumatology (ACR) criteria for RA and had been on a stable dose of MTX for at least six weeks. Patients were randomly assigned to withhold MTX for one week (90 patients) or two weeks (88 patients) after receiving the quadrivalent 2021-2022 seasonal flu vaccine (H1N1, H3N2, B-Yamagata and B-Victoria strains). A control group without an autoimmune disease acted as a reference.
The primary outcome was a positive response at four weeks post vaccination, defined as a four-fold or greater increase in antibody titers against at least two of the vaccine strains. Secondary outcomes were positive response and antibody titers at four- and 16-weeks post vaccination.
The proportion of patients achieving satisfactory vaccine responses were similar in the one- and two-week groups at four weeks and 16 weeks (69% versus 75% and 69.6% versus 70.3%, respectively). The vaccine responses in the RA patients and controls were also similar.
“Patients and physicians alike do not often know what to do with methotrexate when a vaccination, including the annual flu vaccine or novel COVID-19 vaccines, is required. It was relieving to find out that skipping methotrexate for one week is as effective as skipping it for two weeks to improve vaccine response with no increase in disease flare risk,” Dr. Park says. “But it is not clear yet whether skipping methotrexate for one week improves response to other vaccines.”
The next step, Dr. Park says, is to see if this approach can be applied to other DMARDs and vaccines.
More information:
Conference abstract
Source: Read Full Article
