While prior research and analysis have evaluated methods of outpatient labor induction (also known as cervical ripening), the specific approach with the highest efficacy and safety remains uncertain. More than a quarter of all labors in the United States required induction in 2018, according to the National Center for Health Statistics, and will likely continue to rise in the future. A new study by Mount Sinai researchers, published in the American Journal of Obstetrics and Gynecology, aims to identify the most effective and safest cervical ripening strategy.
Unlike previous research that were limited to comparing outpatient vs. inpatient inductions or a one-to-one method comparison, this study is among the first to rank a variety of pharmacologic and mechanical labor induction methods used outside a hospital setting, ranging from commonly used prostaglandin medications to alternative supplements and acupuncture.
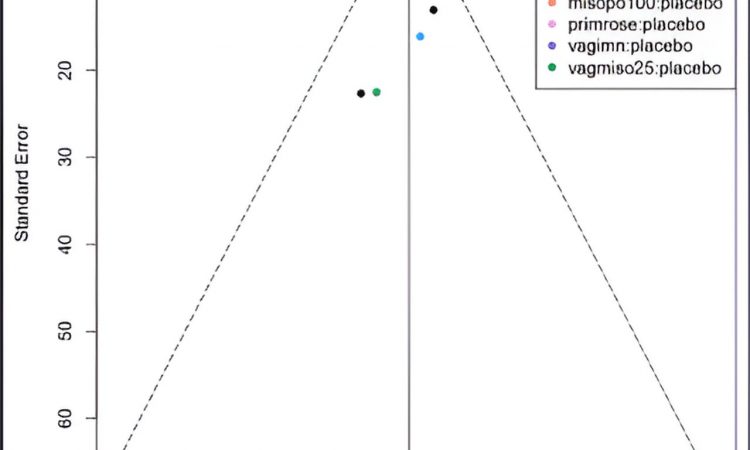
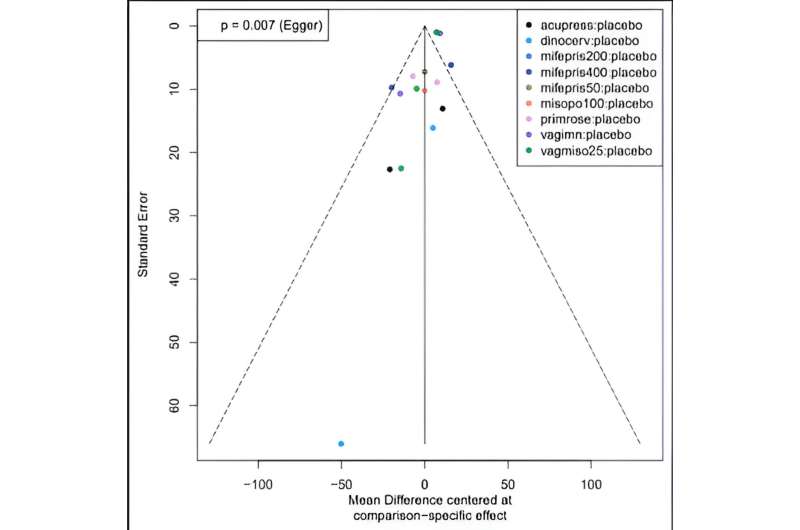
The researchers conducted a systematic review and network meta‐analysis using data from more than 40 randomized, controlled trials with almost 6,100 participants studied in the outpatient setting. The team performed analyses to compare the efficacy of various methods and performed ranking strategies to determine the most effective method. They also assessed the amount of time from labor intervention to delivery, cesarean delivery, need for additional induction methods, a cervix score, Apgar scores (the condition of the newborn immediately after birth), and uterine hyperstimulation, or complications as a result of the induction.
The researchers found that compared with other available labor induction methods, 25 mcg of the medication misoprostol applied vaginally resulted in the shortest time from medical intervention to delivery. This approach did not increase the likelihood of cesarean delivery, need for additional ripening methods, low Apgar scores, or hyperstimulation. Among the effective methods, the team also found that taking 50 mg of mifepristone by mouth was associated with the lowest risk of cesarean delivery. Acupressure, primrose oil, and castor oil were least effective in reducing the time from labor intervention to delivery and cesarean delivery rates.
This latest research provides additional efficacy and safety data for labor induction methods performed in an outpatient setting—which could potentially reduce patient time in the hospital and enhance hospital efficiency in use of resources and staffing. The data confirms the safety and efficacy of outpatient induction using 25mcg of the medication misoprostol, commonly used in the hospital to induce labor. Select patients may be able to start this induction approach at home, requiring less time in the hospital and reducing their medical costs.
Said Mount Sinai’s Dr. Rachel Meislin of the research: “We are excited to add to the growing body of literature regarding the safety of outpatient induction of labor. It is our hope that our findings will contribute to current induction practices.”
Researchers from the University of Missouri-Kansas City School of Medicine and University of Florida College of Medicine contributed to this study.
More information:
Gustavo Vilchez et al, Outpatient cervical ripening and labor induction with low-dose vaginal misoprostol reduces the interval to delivery: a systematic review and network meta-analysis, American Journal of Obstetrics and Gynecology (2023). DOI: 10.1016/j.ajog.2022.09.043
Journal information:
American Journal of Obstetrics and Gynecology
Source: Read Full Article