To help patients manage chronic, often debilitating pain, physicians frequently prescribe medications as first line therapy, although treatment guidelines often call for non-pharmacologic approaches.
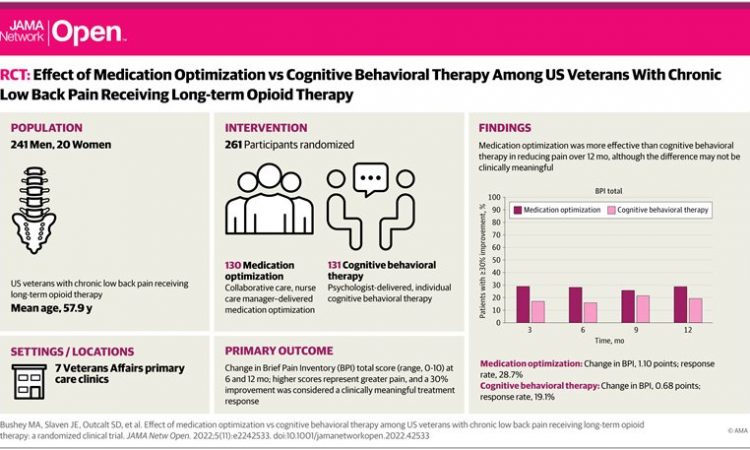
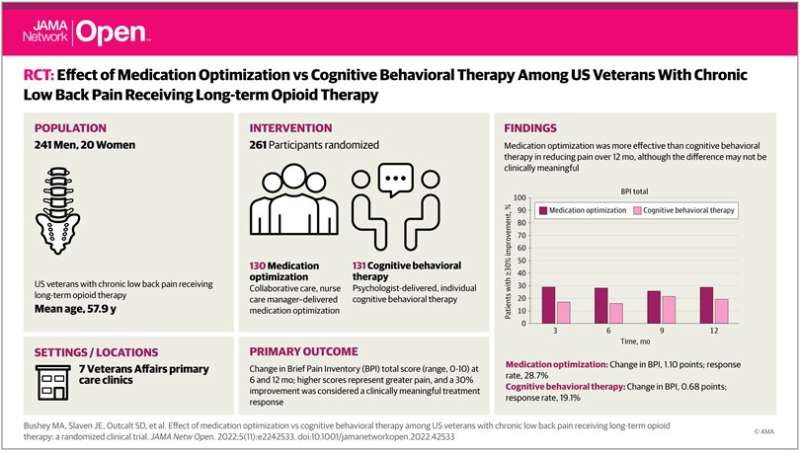
One of the first studies to compare the effectiveness of the two approaches in low back pain patients already on long-term opioids has found that pain improvement was somewhat greater with nurse-delivered medication management than with psychologist-delivered cognitive behavioral therapy.
Although the difference in pain relief was perceived as significant by patients, it was modest in magnitude. The researchers, from the U.S. Department of Veterans Affairs, Regenstrief Institute and Indiana University School of Medicine, noted a reduction in opioid use in participants in the medication management arm of the randomized clinical study.
“I think these findings that both optimized medication management—a pharmacologic approach—and cognitive behavioral therapy—a non-pharmacological approach—are beneficial, provide good news for patients and for clinicians,” said VA and Regenstrief Institute researcher Mathew Bair, M.D., M.S., who led the Care Management for the Effective Use of Opioids (CAMEO) study.
“Also, hybrid care delivery—in person and via telephone—involving two-way communications between patients and clinicians—works well for a population that is very negatively impacted by their pain.”
Medication management was enhanced using a nurse care manager who interacted with the patients with chronic back pain, providing care guided by a specially designed algorithm which directed escalation of pain treatment from simple over-the-counter pain medications to more complex and different categories of pain medications, optimizing dose and patient response while minimizing side effects.
In the cognitive behavioral therapy arm of the study, patients were taught non-pharmacologic strategies and skills to help better cope with their pain and focus on capabilities, not disabilities. These efforts included establishing goals, managing flare ups, handling sleep challenges that are common in low back pain and improving communication with their clinicians.
Veterans with chronic low back pain for at least six months, for which opioids had been previously prescribed, were enrolled in the study. Individuals with active substance use disorder were excluded. Nine out of 10 of the 261 study participants were male.
Pain severity and pain interference with life activities were assessed at three, six, nine and 12 months of study participation.
Approximately half of all U.S. veterans live with chronic pain. Lower back pain is the most common type of pain in this population.
“Many veterans who are prescribed opioids for chronic pain still have significant pain. They may also have PTSD (post-traumatic stress disorder), depression or other psychological conditions which can complicate treatment of their chronic pain,” said study co-author and Regenstrief Institute Research Scientist Kurt Kroenke, M.D.
“Nurse care manager delivered optimized pain medication management, adding non-opioids to treatment regimens, should be just as effective or even more effective in the general population than in the veteran population for chronic low back pain and potentially for other chronic pain conditions.”
The findings are published in the journal JAMA Network Open.
More information:
Michael A. Bushey et al, Effect of Medication Optimization vs Cognitive Behavioral Therapy Among US Veterans With Chronic Low Back Pain Receiving Long-term Opioid Therapy, JAMA Network Open (2022). DOI: 10.1001/jamanetworkopen.2022.42533
Journal information:
JAMA Network Open
Source: Read Full Article