Alzheimer’s disease (AD) is the most common form of dementia, a condition in which the individual suffers the loss of cognitive faculties such as thinking, logic, judgment, language, problem-solving, and memory.
.jpg)
Image Credit: Lightspring/Shutterstock.com
It is a progressive condition and is thought to be linked to a reduced number of interneuronal connections in the brain.
Fibrinogen and AD
The brain in a patient with AD is the presence of abnormal proteins within and around the neurons, called beta-amyloid plaques and tau neurofibrillary plaques. The accumulation of these proteins is correlated with synaptic degeneration and cognitive decline.
Earlier studies have demonstrated abnormalities in the complex vascular network of the brain, but scientists have not been able to clarify if the vascular deficit caused the synaptic breakdown or if it only led to inflammation in the nervous system. Both of these conditions end in cognitive deterioration.
A study from the Gladstone Institutes demonstrated that fibrinogen, a key blood coagulation component, is involved in a cascade of events at both molecular and cellular events which lead to the loss of memory storage neurons within the brain. This is the pathophysiological basis of memory loss, according to the researchers.
The fibrinogen comes from the blood within the brain’s blood vessels. It leaks out of the blood, leading to activation of the microglia, which are the brain’s immune cells. This leads to their attack on the neurons at the synapses, causing their destruction.
The study employed cutting-edge technology to generate the first 3D volume images of AD, from humans and mouse experiments. The researchers then manipulated the mice, preventing the leakage of fibrinogen, which in turn kept the brain’s immune cells quiescent. This protected the brain against memory loss.
In a healthy brain, too, the presence of fibrinogen induced the same type of changes as in AD, but without any evidence of amyloid plaques. This was surprising, as amyloid has been the target of many research efforts to find a therapy that works for AD.
These findings lend support to the hypothesis that dementia is caused by two separate mechanisms. Or in other words, the symptoms of AD and vascular dementia could be due to independently operating underlying disease processes.
Vascular and Amyloid Hypotheses
On the one hand, vascular insufficiency causes dementia, as is seen in elderly people following a stroke. On the other hand, AD occurs in people whose brains show the appearance of amyloid plaques.
Alternatively, both could be part of a linked process. Both sets of people show the deterioration of cognitive abilities and when both pathologies are present, the decline in cognition is more profound than for either alone.
How are Amyloid-Beta and Fibrinogen Linked?
The additive effect of fibrinogen in AD could be partly explained by the fact that when amyloid interacts with fibrinogen or its successor, fibrin, increased amounts of fibrin are deposited within the blood vessels of the brain.
The amyloid-fibrinogen interaction leads to the formation of clots that are resistant to the thrombolytic action of tissue plasminogen activator (tPA) when they are formed directly from thrombin.
This resistance to breakdown could be due to the formation of a tighter fibrin network when associated with amyloid, or because amyloid interferes with the binding of plasminogen to fibrin.
In short, the interaction of fibrinogen or fibrin with amyloid could initiate or aggravate the hypoperfusion and inflammation in the brain.
Fibrin build-up interferes with the normal cerebral perfusion and induces microinfarcts, which lead to neuroinflammation, disruption of the blood-brain barrier, and dysfunction of the neurons.
Simultaneously, the amyloid activates fibrinogen, causing more fibrin to be generated via the intrinsic coagulation pathway. Amyloid also activates factor XII which triggers thrombosis, besides increasing the level of inflammation and vascular permeability through other soluble inflammatory mediators like kallikrein and bradykinin.
Fibrinogen-Linked Prothrombotic State in AD
AD patients may have a higher risk of thrombosis, as shown by higher levels of activated factors VII and V, factor V Leiden (a mutant and more degradation-resistant form of factor V), von Willebrand factor, and prothrombin fragments.
Patients with AD were tested for the risk of spontaneous emboli within the cerebral circulation, compared to healthy age-matched controls. A full 40% of them showed such events, vs only 15% in the controls, and this subset showed a faster cognitive decline over the next 6 months.
Again, microbleeds from cerebral blood vessels occur more frequently in AD than with non-AD controls, perhaps due to ischemia-induced hemorrhage.
Research in mice shows that by reducing the fibrinogen levels, the incidence of cerebral amyloid angiopathy (CAA) declines. With CAA, amyloid is deposited around cerebral blood vessels, causing narrowing and ischemia, as well as blood-brain barrier damage. CAA is present in up to 90% of AD patients.
Reduction in the level of fibrinogen also reduces microglial activation and improves cognitive performance in mouse models. On the other hand, AD is associated with a prothrombotic state: there is a higher tendency to form clots, reduced fibrin degradation, increased platelet activation, and higher levels of clotting factors.
Platelet activation might deliver fibrin directly to forming clots, contributing to the formation of resistant clots.
Directions for Future Therapy in AD
The presence of fibrin in cerebrospinal fluid helps distinguish a patient with AD from mild dementia, or non-dementia patients, and is linked with a more severe disease course. These findings could change the way the condition is perceived and treated.
The use of coagulation data in AD patients could be a novel biomarker, and research suggests that the inhibition of fibrinogen effects in AD could be a new therapeutic target.
Since anticoagulant therapy is a challenge in elderly patients, and AD increases the risk of major cerebral bleeds due to the presence of CAA, novel inhibitors that act on the amyloid-fibrinogen interaction could be useful in the therapy of this devastating condition.
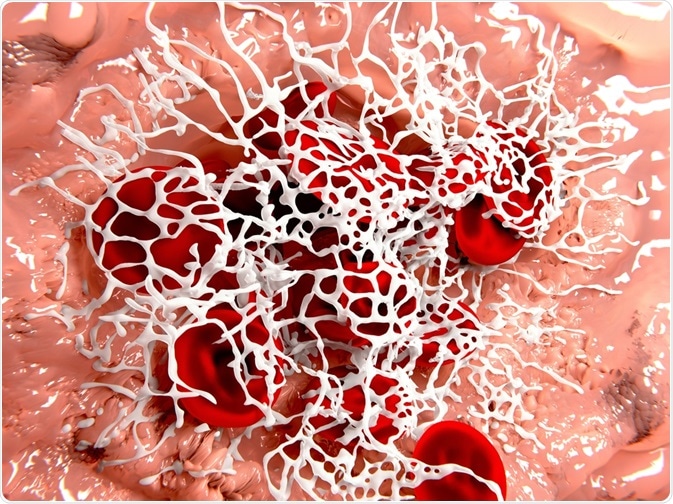
Image Credit: Juan Gaertner/Shutterstock.com
Source
- Strickland, S. (2017). Impact of the Coagulation System on the Pathogenesis of Alzheimer's Disease. Blood (2017) 130 (Supplement 1): SCI-3. https://doi.org/10.1182/blood.V130.Suppl_1.SCI-3.SCI-3. ashpublications.org/…/Impact-of-the-Coagulation-System-on-the
- Suidan, G. L., et al. (2018). Abnormal Clotting of the Intrinsic/Contact Pathway in Alzheimer Disease Patients Is Related to Cognitive Ability. Blood Advances; 2(9): 954–963. doi: 10.1182/bloodadvances.2018017798. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5942003/
- Cortes-Cantelli, et al. (2012). Fibrinogen and Altered Hemostasis in Alzheimer's Disease. Journal of Alzheimer's disease: JAD 32(3). DOI: 10.3233/JAD-2012-120820.
- Merlini, M. et al. (2019). Fibrinogen Induces Microglia-Mediated Spine Elimination and Cognitive Impairment in an Alzheimer’s Disease Model. Neuron. DOI: https://doi.org/10.1016/j.neuron.2019.01.014
Further Reading
- All Alzheimer's Disease Content
- Alzheimer’s Disease | Definition, Causes, Diagnosis & Treatment
- Alzheimer’s Disease Causes
- Alzheimer’s Disease Symptoms
- Alzheimer’s Disease Diagnosis
Last Updated: May 22, 2020

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
