Testing, tracking, tracing, and isolating (TTTI) quickly and on a large scale have proven essential to public health policy responses during the coronavirus disease 2019 (COVID‑19) pandemic. Different kinds of COVID-19 tests have been developed, and each has its pros and cons. Effective testing strategies can combine different tests to achieve complementarity, given their respective advantages and disadvantages.
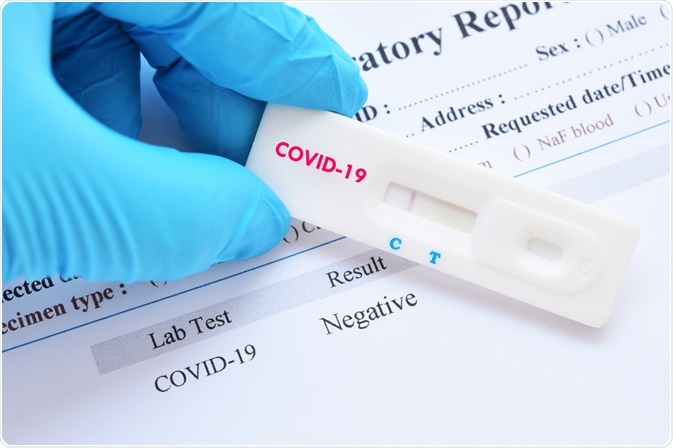 Image Credit: Jarun Ontakrai/Shutterstock.com
Image Credit: Jarun Ontakrai/Shutterstock.com
Types of Covid-19 test
There are two types of COVID-19 test designed to detect an active infection, and these may be divided into molecular tests and rapid antigen tests. A third kind of test, the antibody test, can be used at any time. The RT-PCR and the LFT are different antigen tests and are covered below (1 and 2), followed by a brief look at the antibody test (3), designed to discover a previous encounter with the virus.
RT-PCR
The Reverse Transcriptase – Polymerase Chain Reaction (RT-PCR) is the most well-established technique available and is used to screen for the presence of RNA, which is discernible in the early phase of infection ––before the body has had a chance to manufacture antibodies to the infection. The test works by amplifying the RNA molecule by reverse transcriptase (or DNA polymerase may also be used) to enable detection. It is a highly specific and sensitive test, although results are slower to obtain because samples are sent away to the lab to obtain a result. The high cost of this kind of test has limited its use on a grand scale. Other disadvantages include:
- Positive results different to interpret
- Limitations on supply of essential testing materials ––nasal swabs, reagents, transport media
- Long lead times (in addition to lab processing time) due to the logistics of transporting samples etc.
Point of care RT-LAMP test
The RT-LAMP test is like the RT-PCR test but may be used for point of care testing with no requirement to send the sample to the laboratory, therefore, negating the disadvantage of a long lead time.
CRISPR-based test
This type of test works by identifying a sequence of SARS-CoV-2 RNA and cutting apart any nearby single-stranded RNA. The cuts result in a separately introduced fluorescent particle being released into the test solution that may be subsequently detected using laser ––thereby signaling the presence of genetic material.
Rapid antigen test
These tests are nowadays widely known as the lateral flow test (LFT). This kind of test was developed when the pandemic was well underway, and though less reliable than the RT-PCR test, it has the advantage of being simple and quick to use, offering a rapid test result on a more cost-effective scale.
Antibody test
These serological tests cannot be used to detect current COVID-19 infection but instead to say whether a person has had the infection in the past. These tests are important in the understanding of infection rates in a population and are of epidemiological value. This kind of test is also useful given that many people are asymptomatic for the virus and thus may have been infected without knowing. Antibody testing has been used to detect an immune response in people vaccinated against SARS-CoV-2.
This kind of test requires a sample of blood to be taken from patients rather than a simple swab. The tests come in many forms, from the complex and lab-based (e.g., ELISA tests) to the simpler rapid-tests used at the point of care.
Although these tests play an important role in epidemiology and vaccine development, given they are unsuitable for detecting current, active viral infections, they play no role in implementing TTTI strategies. Finally, just how long vaccine-induced immunity will last is at present unclear to scientists. As the threat of new variants looms large, the need for booster vaccinations is an ever-present prospect.
Which test and when?
The pros and cons of the different testing strategies mean the most appropriate method should be selected according to the circumstances. These should depend on the objectives for carrying out a test in the first instance. The given objectives are:
- Clinical care need ––in which the accurate diagnosis of patients is required to inform clinical decision making
- TTTI strategies ––accurate diagnoses for confirming or disconfirming suspected cases, e.g., because a person was symptomatic or else encountered someone who tested positive for the virus
- Epidemiological monitoring of specific populations ––e.g., groups of people such as in nursing homes, schools and universities, companies, geographic localities
There is not one testing strategy that is effective across all the three given scenarios above. But there are certain advantages to using a given test according to a specific situation. For example, the use of rapid antigen testing has been linked with air travel to ensure that only those who test negative are eligible to travel and as a means for deciphering the need to quarantine. Ultimately, great care should be taken when choosing which COVID-19 test to take to ensure the safety of yourself and those around you.
References
OECD. (2020). Testing for COVID-19: How to best use the various tests? OECD Policy Responses to Coronavirus (COVID-19), OECD Publishing, Paris, https://doi.org/10.1787/c76df201-en
Further Reading
- All Coronavirus Content
- Serological testing for COVID-19
Last Updated: Sep 1, 2021

Written by
Dr. Nicola Williams
I’m currently working as a post-doctoral fellow in the History of Science at the Leeds and Humanities Research Institute (LAHRI), at the University of Leeds. Broadly speaking my research area falls within the remit of the history of biology and history of technology in the twentieth century. More specifically I have specialist knowledge in the areas of electron microscopy and cellular and molecular biology, women in science and visual culture.
Source: Read Full Article
