Aside from an increased vulnerability of being infected by SARS-CoV-2, cancer patients can also experience more severe complications of COVID-19 and/or their prognosis can be indirectly affected by delaying treatment.
 Image Credit: Namomooyim / Shutterstock.com
Image Credit: Namomooyim / Shutterstock.com
As of January 18, 2021, the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infected over 95 million people around the world and was responsible for the death of over 2 million people.
The scientific understanding of SARS-CoV-2 has greatly improved since its initial discovery in December of 2019; however, there remain a number of risk factors that increase an individual’s susceptibility to this virus. Some of these risk factors include, but are not limited to, the male sex, chronic obstructive pulmonary disorder (COPD), hypertension, obesity, several cardiac comorbidities and cancer.
Increased risk of infection
In addition to those mentioned, individuals with cancer are also more vulnerable to infection by SARS-CoV-2 as a result of their systemic immunocompromised state. In fact, it has been estimated from several supporting studies that, as compared to the general population, cancer patients have a hazard ratio of 3.56 when it comes to the coronavirus disease 2019 (COVID-19). One study found that up to 4% of COVID-positive patients had an underlying diagnosis of cancer and that cancer patients who became seriously ill or died as a result of having COVID-19 accounted for up to 20% of the COVID-positive patients in this study.
Of note, however, is that COVID-19 does not appear to affect all cancer patients equally, as some studies have found that cancer patients with a subset of certain cancers may be at an even greater risk when it comes to COVID-19.
For example, patients with hematologic, lung or other metastatic malignancies, as well as those who had previously undergone surgical resection procedures, were at a greater risk of getting severely ill following infection by SARS-CoV-2. This same study also found that patients with non-metastatic cancers are at a similar risk of experiencing the severe effects of COVID-19 as the general population.
Age also appears to increase the risk of severe or critical COVID-19 events in cancer patients, as the fatality rate for cancer patients with COVID-19 is significantly greater as the patient’s age increases.
Delayed cancer treatments
The increased vulnerability of cancer patients to COVID-19, particularly to the severe effects of this infectious disease, has led some patients to delay or pause their anti-cancer treatments to reduce their exposure to potentially infected people.
In one retrospective study, 9.1% of lung cancer patients decided to delay their cancer treatments, of which 80% chose to delay treatments themselves rather than as a result of a clinician or family request.
Another study found that a delay of four weeks in all forms of cancer treatment can increase patient mortality and that delays greater than four weeks can be even more detrimental. While the anxieties surrounding the current pandemic are understandable, it is generally recommended that cancer patients continue their standard treatment regimen in order to prevent a worsening of their prognosis.
Complications of COVID-19 in cancer patients
One of the most pressing concerns for clinicians is the potential cardiovascular complications that can arise in cancer patients who have also been infected with SARS-CoV-2.
Some of the most common cardiovascular complications to arise in COVID-19 patients in the general population include embolism, stroke, arrhythmias and other cardiac injuries.
Since cancer, as well as several different cancer treatments, are also associated with an increased likelihood of inducing certain cardiovascular complications in patients, the combined effect of this with those associated with COVID-19 can be devastating.
Some of the specific complications that can be further exacerbated by COVID-19 in cancer patients include blood stasis, vascular wall damage and hypercoagulation states, all of which can increase the chance of thrombosis.
While the exact mechanism responsible for this synergy between COVID-19 infection and cancer that leads to these cardiovascular complications are not fully understood, it is generally believed that a hyperinflammatory reaction to these two conditions can promote dysfunction in the cardiovascular systems of these individuals.
The renin-angiotensin-aldosterone system (RAAS)
Another area of concern in COVID-19 positive cancer patients is the renin-angiotensin-aldosterone system (RAAS). In cancer biology, RAAS plays a key role in the remodeling of the tumor microenvironment, as well as in supporting the growth and metastasis of cancer cells throughout the body. Likewise, COVID-19 also alters the normal function of the RAAS through its utilization of the angiotensin-converting enzyme 2 (ACE2) receptor, which the virus uses to gain entry into cells.
By reducing the normal expression of ACE2 from cell surfaces, the SARS-CoV-2 virus causes an imbalance in RAAS and thus further disrupts normal endothelial function throughout many tissue types and organs in the body. Since certain cancers might be treated with ACE inhibitors, further dysregulation of the RAAS system by COVID-19 may lead to more severe adverse effects of this treatment regimen.
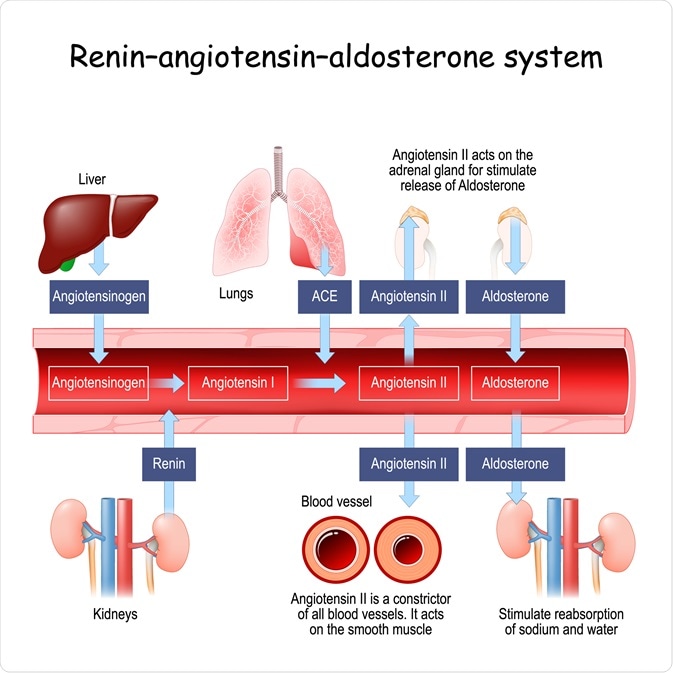 Diagram of the renin-angiotensin-aldosterone system (RAAS). Image Credit: Designua / Shutterstock.com
Diagram of the renin-angiotensin-aldosterone system (RAAS). Image Credit: Designua / Shutterstock.com
Key biomarkers in COVID-19 cancer patients
Several biomarkers have been used to monitor the severity of COVID-19 in cancer patients, which include, but are not limited to C-reactive protein (CRP) and interleukin-6 (IL-6).
CRP is typically used to detect endothelial dysfunction during inflammatory events, such as viral infections like COVID-19 or chronic cardiovascular diseases. When used to monitor COVID-19 in positive patients with a history of leukemia, myeloma and lymphoma, CRP levels of more than 10 mg/dl have been found to significantly correlate with a greater likelihood of COVID-19 related death.
IL-6 is a proinflammatory cytokine that is not only involved in the immune system’s response to infection, as it often contributes to a fever and other innate responses, but this substance also plays a role in how much CRP is released from the liver.
Although the blocking of IL-6 is often beneficial in cancer patients when combined with certain conventional therapies, the blocking of this cytokine in COVID-positive cancer patients can instead cause severe side effects. Some of the more notable side effects of blocking this pathway can include an enhanced immunocompromised state, a greater chance that the patient acquires a secondary infection or other types of off-target effects.
References
- Gupta, K., Gandhi, S., Mebane III, A., et al. (2021). Cancer patients and COVID-19: Mortality, serious complications, biomarkers and ways forward. Cancer Treatment and Research Communications 26. doi:10.1016/j.ctarc.2020.100285.
- Hanna, T. P., King, W. D., Thibodeau, S., et al. (2020). Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ 371. doi:10.1136/bmj.m4087.
- Williams, M., Mi, E., Le Calvez, K., et al. (2020). Estimating the Risk of Death from COVID-19 in Adult Cancer Patients. Clinical Oncology. doi:10.1016/j.clon.2020.10.021.
Further Reading
- All Coronavirus Disease COVID-19 Content
- What Mutations of SARS-CoV-2 are Causing Concern?
- Can Pets Get COVID-19?
- An Overview of the SARS-CoV-2 Vaccines
- Repurposing Drugs for COVID-19
Last Updated: Jan 21, 2021

Written by
Benedette Cuffari
After completing her Bachelor of Science in Toxicology with two minors in Spanish and Chemistry in 2016, Benedette continued her studies to complete her Master of Science in Toxicology in May of 2018.During graduate school, Benedette investigated the dermatotoxicity of mechlorethamine and bendamustine, which are two nitrogen mustard alkylating agents that are currently used in anticancer therapy.
Source: Read Full Article
