A vitrectomy is a surgical procedure that may be carried out for a number of reasons:
- improving vision in patients experiencing complications from diabetes
- removing foreign bodies from the eye in cases of trauma
- taking a biopsy to diagnose infections or diseases
- as part of other operative procedures on the retina
The aim of the procedure in most cases is to remove the vitreous humour to allow access to other parts of the eye.
The vitreous humour is usually a transparent, gelatinous substance inside the eye, found behind the iris and the lens, and in front of the retina. Its only purpose is to give volume to the eye.
There are two different types of vitrectomies, posterior pars plana vitrectomy and anterior vitrectomy.
Posterior pars plana vitrectomy
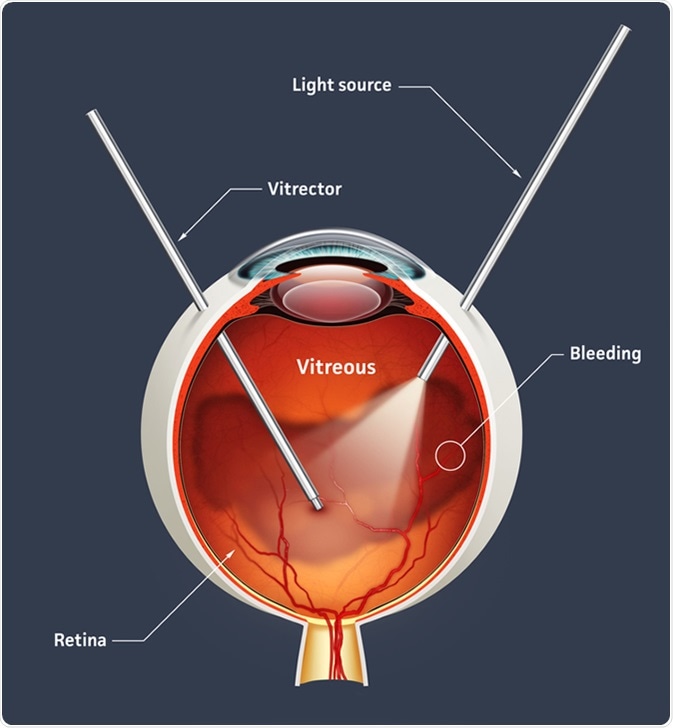
This type of vitrectomy is carried out by a retina specialist. This procedure involves removing the vitreous gel from the eye through the pars plana, the region of the eye that is thought to have no function in the post-fetal period and as such is thought to be the safest point of entry into the eye. Surgical instruments are also introduced into the eye through the pars plana.
The vitreous jelly is dissected and then peeled or sucked out through small 1mm cuts made into the white of the eye. Any necessary repairs to the retina are carried out, as well as removing any foreign bodies, or, in the case of surgery to treat complications of diabetes, leaking blood vessels are sealed.
Anterior vitrectomy
Anterior vitrectomies are carried out when vitreous gel leaks through the pupil and into the anterior (front) chamber of the eye. Eye trauma, cataracts of the lens, and corneal or glaucoma surgery, can cause this to occur. Anterior vitrectomies aim to minimize the risk of developing future problems due to leaking vitreous fluid, and to improve visual recovery.
Vitrectomy procedure: steps
Before the vitrectomy is done, pre-operative assessments are carried out. A full history is taken, covering both general and eye health, and details of medications prescribed for other conditions are discussed. Checks to ensure that anesthesia may be safely used on the individual patient will also be carried out. General anesthesia is usually used for vitrectomy procedures, but local anaesthetic can also be used if precisely placed.
Once a patient is underneath anesthesia, the eye is kept open with forceps. The doctor will make a small (1mm) incision, and cut through the pars plana, also known as the sclera or the white of the eye. A surgical microscope that allows a wide view of the inside of the eye, along with a magnified view, is inserted. Fiberoptic cables are also used to illuminate the inside of the eye. These instruments are inserted via separate openings. The vitreous fluid is then extracted using a vitrectomy probe and any retinal problems are treated at the same time. In diabetics, leaking blood vessels are laser-coagulated at this time.
The procedure usually takes several hours.
As vitreous jelly does not reform by itself, it is necessary to replace it with one of the substances below:
- A gas bubble that is absorbed naturally over 2-3 weeks
- Air that is absorbed within 24-36 hours
- A blend of gas and air
- An oil or heavy liquid that is surgically removed later
The chamber that was once filled with vitreous jelly will be filled naturally with aqueous humour after the gas and air have been absorbed.
Recovery from vitrectomy surgery
After vitrectomy surgery, vision will be blurred for several weeks. The eye will be sensitive and swollen, and improvement may not be seen until two weeks after the surgery.
If gas or oil has been used to replace the vitreous jelly, some patients are told to position their head in a downward tilt to ensure that the gas or oil is against the treated area of the retina, as gas will float to the top of the eye. Patients are asked to do this for around 4 to 14 days, for 50 minutes per hour, although this can change depending on the reason for the surgery. To make this more comfortable, neck pillows can be used. It is also advised that patients lie on their front when sleeping. All of these measures help the retina to heal in the right place.
Complications from vitrectomy procedures
Cataracts are known to occur after vitrectomies. The formation of cataracts has been linked to high oxygen levels in the proximity of the lens, which isn’t usually exposed to a lot of oxygen. It is hypothesized that the substances used to replace vitreous fluid do not keep oxygen away from the lens as efficiently as the natural vitreous fluid does. Retinal damage can also occur when air is inserted into the eye to replace the vitreous fluid.
If patients experience a significant decrease in vision quality, or increase in colored discharge, pain, swelling, light sensitivity or redness, emergency medical attention from an eye hospital should be sought.
Some patients may experience high pressure in the eye, which is treated with eye drops. Increased pressure in the eye can cause double vision and pain.
There is also a risk of infection, as with any surgical procedure. Infections will usually be treated with antibiotics.
Other complications include:
- Bleeding in the eye
- Damage to the lens
- Problems with eye movement
- Inflammation
- Retinal re-detachment
- Drooping eyelid
- Distorted or blurred vision
Sources
- https://www.asrs.org/patients/retinal-diseases/25/vitrectomy
- www.ouh.nhs.uk/patient-guide/leaflets/files/100322vitrectomy.pdf
- www.guysandstthomas.nhs.uk/…/vitrectomy.pdf
- www.reviewofophthalmology.com/…/complications-of-vitreoretinal-surgery
Further Reading
- All Vitrectomy Content
Last Updated: Feb 26, 2019

Written by
Lois Zoppi
Lois is a freelance copywriter based in the UK. She graduated from the University of Sussex with a BA in Media Practice, having specialized in screenwriting. She maintains a focus on anxiety disorders and depression and aims to explore other areas of mental health including dissociative disorders such as maladaptive daydreaming.
Source: Read Full Article
