Radiotherapy can effectively reduce or even eliminate some tumours; others, however, show enduring resistance. Considering the potentially harmful side effects of radiotherapy, clinicians agree that it is paramount to be able to determine if a patient will benefit from radiotherapy before exposing them to any of the associated risks.
Despite significant efforts to develop biomarkers that can assess the potential efficacy of radiotherapy treatment for individual patients, there is currently no established diagnostic test that can provide a clear answer.
To address this urgent need, a multidisciplinary team working at the Champalimaud Centre for the Unknown in Lisbon, Portugal, developed a novel assay for quick radio-sensitivity diagnosis. Depending on the success of upcoming clinical trials, this assay may become a standard personalized medicine tool within a few years. Their results were published today (December 17th) in the scientific journal EBioMedicine, a biomedical open access journal, published by The Lancet.
The four days assay
The team is already known for having established a successful chemotherapy-sensitivity assay, based on transplanting tumor cells into zebrafish and using these avatars for treatment testing. Their results stand now at 85% success rate for predicting how tumors will respond to specific drugs.
Moving into radiotherapy response testing has presented the team with a new set of challenges, which they met by combining the expertise of clinicians, physicists and biologists. The group decided to establish the assay focusing on colorectal cancer, which is the third most common cancer worldwide. “Radiotherapy sensitivity is particularly important for rectal cancer,”‘ says Rita Fior, one of the lead authors of this study. “In the majority of cases with locally advanced disease, the standard approach is first to administer chemo-radiotherapy and then perform surgery to remove the tumor.”
According to Nuno Figueiredo, Head of the Champalimaud Surgical Center, the new assay has the potential to have a tremendously positive impact on patients’ lives. “Some tumours may be highly radio-sensitive, leading to a reduction of tumour size or even elimination of the tumour altogether. This allows for a more conservative ‘watch and wait’ approach in which radiotherapy may effectively postpone or even prevent invasive surgery. On the other hand, if the tumour is radio-resistant, the optimal solution, which is surgery, can be implemented without further delay.”
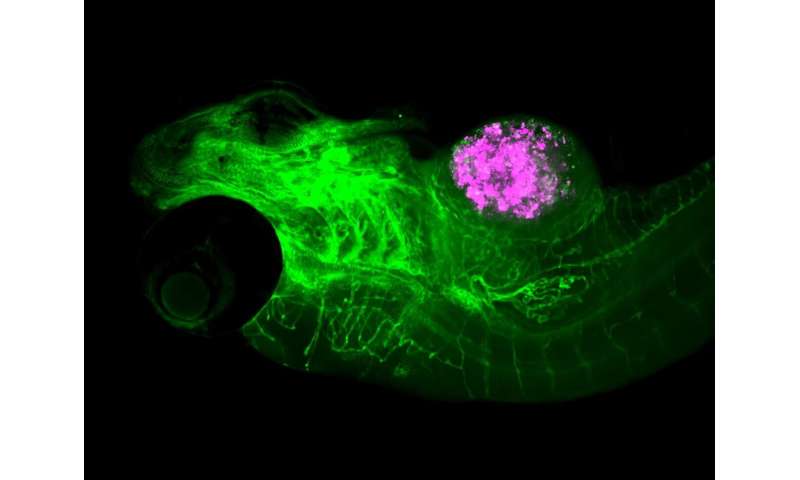
To establish the radiotherapy assay, the team first transplanted tumor cells from human colorectal cancer cell-lines into zebrafish, thereby creating the zebrafish “avatars.” Specifically, they focused on two types of cells—radio-sensitive and radio-resistant. Radiation was delivered to the avatars using the same equipment (linear accelerator) applied for the treatment of cancer patients.
The results were promising: ” We were able to decisively say which tumor cells had responded to the treatment after just four days. The full set of analysis took an additional eight days. This was very exciting, as it is a very fast timescale that will work well for clinical application,” points out Susana Ferreira, a biologist that co-authored the study.
From the lab to the clinic
After establishing the radio-sensitivity assay, the team conducted a “proof of concept” experiment, where they tested it in a clinical setting. They ran the assay on cells derived from biopsies of two patients that were recently diagnosed with rectal cancer and were about to undergo treatment. The results were robust: “the response of the zebrafish avatars perfectly mirrored the response of the patients,”‘ says Bruna Costa, another co-author of the study.
Oriol Parés, a radiation oncologist who participated in the project, stresses the importance of establishing a radio-sensitivity assay. “There is a global investment towards finding biomarkers that could predict the response of patients to chemo and radiotherapy. This preliminary clinical trial yielded promising results, supporting the prospect of using this assay as a cost-efficient test with timely results. It also corresponds with a modern approach in medicine, which we apply here at the Champalimaud Clinical Centre, to personalize treatment with the goal of optimizing results for each individual patient.”
“This is a great example of what can be achieved in cancer clinical research,” adds Miguel Godinho-Ferreira, a researcher involved in the study. “At the Champalimaud Centre for the Unknown, not only do we gather patients, clinicians and scientists under the same roof, we also have the financial support to bring the most recent advances of research to cancer patients. I cannot wait to have our assay helping people suffering from this disease.”
Source: Read Full Article
