The term “microbiome” is shorthand for the vast and still largely unexplored worlds of bacteria, viruses, fungi and other microorganisms that inhabit every corner of the planet. Bacteria form tiny ecosystems side by side with our own cells on our skin, in our mouths and along our airways and digestive tracts, as well as on all the surfaces we interact with—including our homes, workplaces, and hospitals, and the air, water, and soil.
These microbes are so impactful that some researchers consider them to be a separate organ, which shapes our metabolism, susceptibility to allergic and inflammatory diseases, and even responses to medical treatments. But scientists at the University of Chicago and other institutions around the world are just beginning to fully understand the role that bacteria play in our health.
What is a microbiome?
In 1675, Dutch haberdasher Antonie van Leeuwenhoek peered through a microscopic lens at some lake water and saw that it was teeming with life. Along with tufts of green algae, he saw thousands of tiny creatures he dubbed “animalcules.”
Centuries later, we now know that Leeuwenhoek’s animalcules inhabit every surface, nook and cranny of the planet. The term “microbiome” was coined to describe the collective community of bacteria, viruses, fungi and other microbes that colonize a particular space or ecosystem—for example, a microbiome of the soil, or a microbiome of a body of water. Indoor spaces like homes, offices and hospitals also have distinct microbiomes, as do all the surfaces and objects within. And most multicellular life forms have their own microbiome—a collection of microbes that are co-dependent, adapting to and taking advantage of the conditions presented by the host. Microbiomes can have a profound impact on the host’s biology and health.
Scientists at the University of Chicago and other institutions around the world are working to understand and catalog the microbiome, and to apply these insights to interventions and biotherapeutics to maintain health and to prevent and treat disease.
Why is the gut microbiome so important?
The human body has several distinct microbiomes—on the skin, in the mouth and in our airways—but the most consequential one for health is in the digestive system, commonly called the gut microbiome. The millions of microbes in the large intestine constantly exchange chemical signals with the body’s cells and help digest nutrients. These bacteria form a mutualistic or symbiotic relationship with the body and contribute to the normal functioning of the digestive system and other bodily organs and systems, so much so that some researchers see the gut microbiome as its own distinct organ.
This microbiome relies on a careful balance of certain types of bacteria that provide the services the body needs. Sometimes, one type of bacteria is found lacking or another type becomes more abundant than others, which can throw the system out of whack. This is called dysbiosis, which can lead to several health problems.
How does the gut microbiome impact human health?
In the 1980s, UChicago alum Jeffrey Gordon, MD’73, a gastroenterology researcher working at Washington University School of Medicine in St. Louis, began studying the gut microbiome to understand this nuanced relationship between microbes and their hosts. Gordon and his team were studying intestinal development, exploring the chemical signals that cells exchange with each other.
In one groundbreaking experiment, Gordon’s group transplanted gut microbes from both genetically obese mice and lean mice into a group of germ-free mice, which were specially raised to have no microbes. Despite all the mice eating the same diet, the mice who received microbes from obese mice gained more weight. At the same time, Gordon and his colleagues also showed how the gut microbiome of obese humans changed as they consumed low-calorie diets and lost weight. Gordon became known as “the Father of the Microbiome” for this work, which renewed interest in the links between the gut microbiome and human health.
The microbiome also plays a role in digestive diseases. In 2012, University of Chicago gastroenterology researcher Eugene B. Chang published a study showing how the high-fat, high-calorie diet common in Western countries may contribute to the rise in inflammatory bowel disease, or IBD, over the past century. Chang’s team discovered that highly saturated fats typically consumed in a Western diet alter the composition and functional properties of bacteria in the intestines. These changes can disrupt the normally beneficial mix of microbes and lead to the emergence of microbes that trigger inflammation and damage the intestine. Later, his group also showed how such a calorie-rich, Western diet can induce the expansion of specific microbes that promote the digestion and absorption of high-fat foods. Over time, it’s thought the steady presence of these microbes can contribute to over-nutrition and obesity.
Antibiotics can also decimate bacteria in the gut. Chang’s lab has shown that when mice that are genetically susceptible to IBD were given antibiotics late in pregnancy, their altered gut microbiome was transferred to their offspring, resulting in interruptions to immune development and much higher incidence of colitis. In a later mouse study, they also showed how restoring a single microbial species, Bacteroides, at the right development point could repair the antibiotic-damaged microbiome, restore proper immune development, and significantly lower the risk for developing colitis later in life.
How does the gut microbiome affect allergies?
The gut microbiome also plays a key role in the development of food allergies. Food allergies occur when the body triggers an overreactive, damaging immune response to certain foods, such as peanuts, milk or shellfish. Some studies have hinted that modern lifestyle practices like low-fiber diets, overuse of antibiotics, cesarean births, and formula feeding can disturb the body’s natural bacterial composition.
In 2014, a team led by immunologist Cathryn Nagler at UChicago showed that the presence of one common class of bacteria called Clostridia can protect against the development of food allergies by strengthening the gut barrier to minimize exposure to allergens. Later in 2019, Nagler and colleagues showed that a particular species of Clostridia, which is abundant in infants, can protect against the development of an allergy to cow’s milk. Most recently, Nagler and her collaborators at Stanford studied twin pairs where one twin had a food allergy and the other did not. They found that the twins without food allergies tended to have more of the protective Clostridia bacteria in their guts and maintained it throughout their lifetime.
What other aspects of health are related to the microbiome?
Research is underway on how the microbiome contributes to other health conditions, including kidney stones, Alzheimer’s disease, Crohn’s disease, colon cancer, diabetes, celiac disease, allergies, heart disease, asthma, acne, liver disease, Alzheimer’s disease, multiple sclerosis, depression, anxiety, rheumatoid arthritis, psoriasis, stroke, and even disrupting the body’s circadian rhythms and sleep cycles.
It can even affect how we develop; UChicago Prof. Erika Claud showed the importance of the early-life microbiome in brain development.
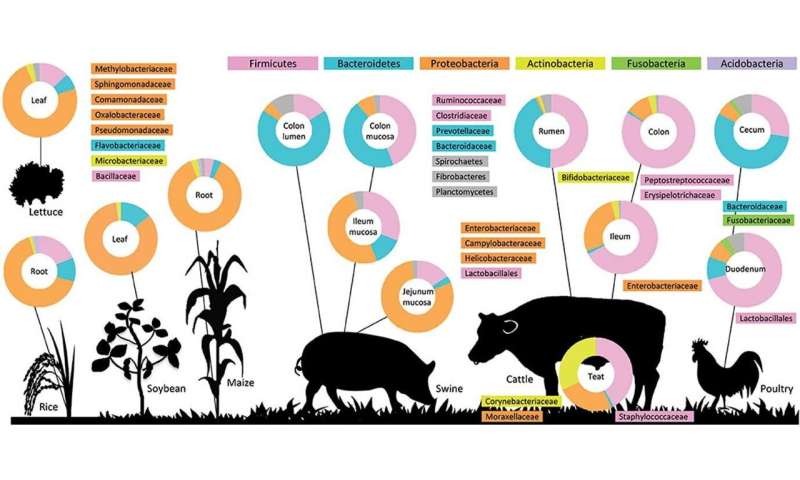
How does the environment affect the microbiome?
Studies have connected the environment where someone lives to differences in their body’s microbiome, which in turn affects health.
For example, in 2016, Carole Ober and Anne Sperling showed how the differences between two farming communities, the Amish of Indiana and Hutterites in South Dakota, are associated with changes in immune cells that protect one group of children from developing asthma but not the others. The Amish and Hutterites have similar genetic ancestry and share similar old-fashioned lifestyles and customs. Their farming practices differ, however. The Amish live on single-family dairy farms in close contact with cows and horses. The Hutterites live on large communal farms with modern, industrialized machinery that limits daily contact with farm animals.
The research suggested that closer contact with the animals and their microbes via household dust gave Amish children more blood cells that fight infections and fewer that promote allergic reactions. Amish children have one half the average rate of asthma for U.S. children, and a quarter of the rate among Hutterite children.
Can you use the microbiome to treat disease?
All of this research might give the impression that if disruptions of the microbiome lead to disease, one could treat those same diseases by restoring a “healthy” microbiome. That’s the ultimate goal, but many of the early links between the microbiome and health are just correlations—that is, researchers cataloged differences the microbiome of healthy people and those with a disease, but don’t yet understand the details. We still have much to learn about the specific mechanisms and types of microbes that lead to these disruptions.
A common approach to manipulating the microbiome to promote health is through probiotics, or cocktails of bacteria that can restore a proper balance. However, most of the common probiotic supplements sold in drugstores and foods like yogurt likely just pass through the system without properly colonizing the gut. More effective remedies may come in the future: Researchers are working on targeted, precise treatments that interact with the gut microbiome, like the therapeutics Nagler and UChicago biomolecular engineer Jeffrey Hubbell are developing through their academic startup company ClostraBio.
The microbiome can even influence how the body responds to medical treatment. UChicago cancer researcher Tom Gajewski has shown that a higher prevalence of specific strains of bacteria in the gut can improve the response rate for melanoma patients being treated with immunotherapy. These drugs are designed to boost the immune system response to fight cancer, and the presence of these bacteria appears to enhance the potency of immune T-cells as they infiltrate tumors and attack cancer cells. This suggests that probiotics including these enhancing bacteria could someday be used to augment immunotherapy. Similarly, Prof. Eric Pamer showed that cancer patients with greater gut microbiome diversity had higher rates of transplant success.
Scientists are still scratching the surface of the power of the microbiome and its profound influence on our bodies. Much of the ongoing work is being spurred by advances in genetic sequencing technology that can not only catalog the different microbes present in a given environment, but also analyze their gene expression and the proteins and other molecules they produce to understand their activity.
Source: Read Full Article
