Immune responses against Factor VIII, which is used to treat hemophilia A (bleeding disorder), are influenced by the microenvironment of antigen presenting cells. This is the result of a scientific study conducted in cooperation between the Institute Krems Bioanalytics of IMC University of Applied Sciences Krems and the international pharmaceutical company Takeda, which was recently published in the journal Frontiers in Immunology.
In this study, a cell culture model was used to investigate the impact of the microenvironment on factor VIII uptake and processing in antigen presenting cells. The observed alterations in protein processing might have profound effects on immune responses to FVIII. The novel data provide the basis for the development of future FVIII therapies that elicit minimal immune responses in patients.
Hemophilia A is a hereditary bleeding disorder caused by absence or deficiency of active clotting factor VIII (FVIII) in the blood. Patients are therefore treated with FVIII replacement therapy.
A major complication of this therapy is the development of a neutralizing immune reaction in 30% of the patients, thereby rendering the administered FVIII ineffective. Why such a complication occurs in some people while others are spared is not yet clear—and it is precisely this issue that the research group from Takeda and IMC Krems led by Dr. Christian Lubich set out to address.
Adverse immune response
“The experimental design of our cell culture study,” Dr. Lubich stated, “was aimed at taking a closer look at the response of different immune cells in the context of FVIII administration and thereby gaining better insight into the underlying processes.”
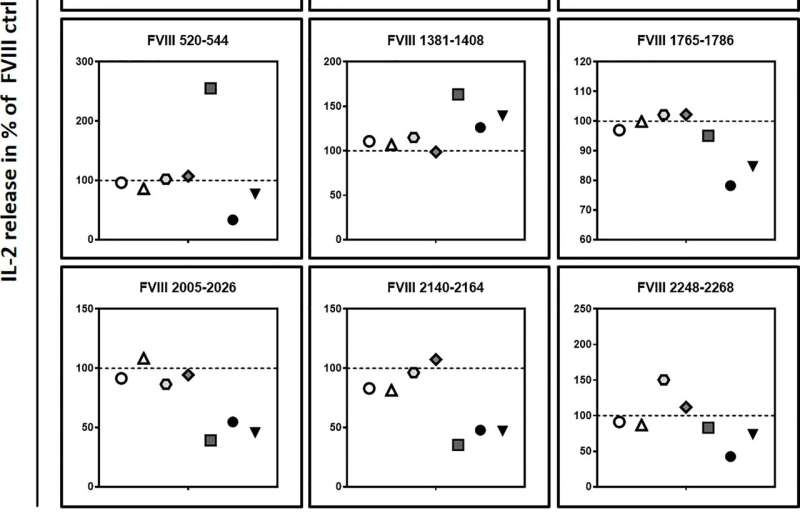
And indeed, the study data suggest a crucial link between the specific microenvironment during FVIII uptake by specific immune cells—so-called antigen-presenting cells (APCs)—and the FVIII proteins (antigens) presented by these cells on their cell surface. Depending on the microenvironment, the composition of these surface proteins differs and thus also influences the specificity of the subsequently activated CD4+T cells, partly resulting in the undesired neutralizing immune response.
New technology
To verify the relevance of the data in vivo as well, it would now be useful to conduct a follow-up study in humans. Dr. Lubich and his team at the Institute of Krems Bioanalytics already have an idea for this, based on a promising new technology: “Immunopetidomics is a pioneering method for investigation of the composition and dynamics of proteins presented by antigen-presenting cells with the aid of mass spectrometry.”
“This method can be used, for example, to determine peptides of a pathogen, a tumor cell or, as in this case, a biotherapeutic agent that elicit an immune response. This platform will therefore not only help to better understand adverse reactions of the immune system to biotherapeutics, but will also enable the identification of important antigens for the development of immunotherapies.”
More information:
Christian Lubich et al, Modulating the microenvironment during FVIII uptake influences the nature of FVIII-peptides presented by antigen-presenting cells, Frontiers in Immunology (2022). DOI: 10.3389/fimmu.2022.975680
Journal information:
Frontiers in Immunology
Source: Read Full Article
