Introduction
The problem
Clinical presentation
Types of Urinary TB
Complications
Diagnosis
Management
References
Further Reading
Introduction
Urinary tract tuberculosis is usually caused by the bacilli spread through the bloodstream from chronic latent pulmonary tuberculosis. In many cases, the condition's occurrence goes unrecognized, mistaken for those coincident symptomatic urinary tract infections (UTIs) by other microbes.
Tuberculosis (TB) is the number 1 killer among infections worldwide. It causes 10 million new cases yearly, with roughly 2 million people dying of this infection. Almost 95% of pulmonary and urinary tract TB come from developing countries (low- and middle-income countries (LMIC).
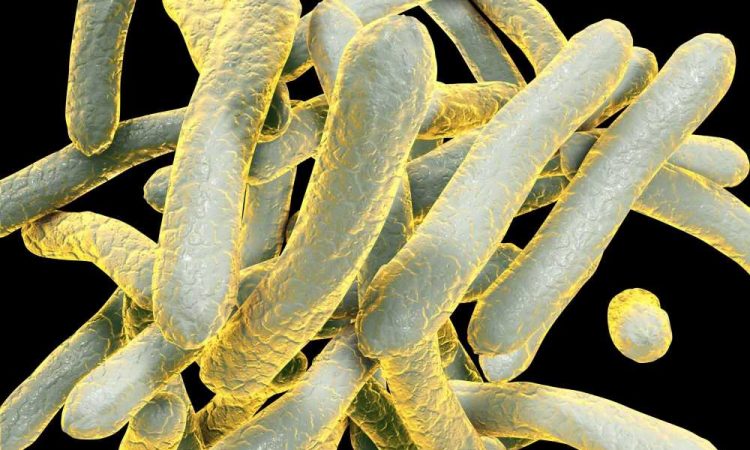
 Image Credit: KaterynaKon/Shutterstock.com
Image Credit: KaterynaKon/Shutterstock.com
The problem
It is worth remembering that the coronavirus disease 2019 (COVID-19) pandemic, which has garnered so much attention and absorbed such a large proportion of research and government funding, has caused roughly the same number of deaths each year over the 2.5 years since it began.
Yet, compared to the over US$ 100 billion spent on the COVID-19 vaccines alone, TB funding decreased by almost a tenth in 2019-20, to US$ 5.3 billion, in the most-affected countries.
In 5% to 45%, TB pathogens involve organs outside the lungs, most often the urinary or reproductive tract. The latter systems are involved after as little as five years or as long as 40 years of latent pulmonary TB in between 2% to 10% of cases.
Urinary tract TB is more common than reproductive tract TB. It is often diagnosed after a significant delay when it has caused complications such as stricture formation in the urethra or ureter or renal failure.
In most cases, it is caused by Mycobacterium tuberculosis. Still, others may be involved in a few cases, such as Mycobacterium bovis, Mycobacterium africanum, Mycobacterium pinnipedii, Mycobacterium microti, Mycobacterium caprae, and the TB vaccine bacillus Calmette–Guérin (BCG).
The bacilli may remain dormant within the urinary tract, having got there via the bloodstream in most cases. However, in some instances, it could be via lymphatic channels or by sexual transmission. Reactivation is more likely to occur in people with diabetes, advancing age, low body mass, immunosuppression due to cancers, other conditions, or kidney failure. The human immunodeficiency virus (HIV) pandemic has led to a resurgence of extra-pulmonary TB.
The pathogen first infects the lung or gut, depending on whether it is inhaled or ingested. This may elicit immune responses that lead to forming of a primary granuloma intended to imprison the mycobacteria or clear them from the host.
These are highly slow-growing obligate intracellular microbes, resulting in a long incubation period before the clinical symptoms appear. Only susceptible hosts develop TB, while others with robust innate immunity appear to resist latent TB despite prolonged or high-degree exposure.
Clinical presentation
The presentation of urinary tract TB varies with the organ affected and the intensity of symptoms. The infection can be asymptomatic as well. Clinical manifestations include constitutional symptoms – fever, loss of appetite, night sweats, and weight loss.
Some UTIs fail to respond to standard antibiotic protocols, with recurrences that appear to be due to antibiotic resistance. The presence of urinary TB should be ruled out in such cases.
 Image Credit: Rattiya Thongdumhyu/Shutterstock.com
Image Credit: Rattiya Thongdumhyu/Shutterstock.com
Types of urinary TB
Urinary TB most commonly affects the kidney. With non-specific presenting features, it may ravage the renal parenchyma and eventually cause obstructive disease of the kidneys, with end-stage kidney failure.
Initially, the cortical renal granulomas formed around the bacilli may remain dormant for decades. The clinical disease begins insidiously with dysuria and hematuria. Interestingly, even though the pathogen seeds both kidneys, only one develops active disease.
This is often characterized by caseating granulomas around the glomeruli. The capillaries of the granuloma break open, allowing the multiplying bacilli to enter the interstitial tissue.
Interstitial TB nephritis is a severe disorder and may cause renal failure. The renal papillae may be destroyed, with subsequent ulceration or abscess formation. Sometimes, pseudotumors form within the kidney and may be confused with renal cancer, leading to the performance of unnecessary nephrectomy.
TB of the ureters is mainly in the lower third, with the following common site being the upper end. It usually accompanies renal TB, which may cause strictures of the tube and thus block urine flow. This may result in hydronephrosis and kidney failure. Hematuria or abdominal pain is more likely with this form.
TB of the bladder is typically secondary to renal TB, though blood-borne or lymphatic dissemination can also occur. It may present as a resistant UTI. It may also cause obstructions due to inflammatory stricture formation, ending in renal failure.
Prostate TB is usually blood-borne but is typically asymptomatic at the onset. This is followed by symptoms associated with voiding urine, finally causing dysuria, frequent nocturnal urination, pelvic pain, and/or sexual problems.
Complications
Urinary TB may be complicated by other infections, strictures, or fistula formation due to fibrosis, renal failure, hypertension due to kidney damage, prostate abscess, and a reduced ability to hold urine due to lower bladder capacity.
Diagnosis
Urinary TB is diagnosed by the history and physical examination with specific radiological and laboratory findings. The primary evidence is a positive isolate for M. tuberculosis from the clinical samples from the urine, prostate massage fluid, or biopsy.
Methods include smear microscopy to detect the bacilli, LED-based fluorescent microscopy, Mycobacterial culture from urine samples, and the Xpert MTB/RIF assay. Culture is done on solid or liquid media, taking 6-8 weeks vs. ten days for the results, respectively.
For this reason, the automated liquid Mycobacteria Growth Indicator Tube (MGIT) culture is the WHO gold standard for TB confirmation. Culture allows for identifying the bacillus, drug sensitivity testing, its good performance characteristics with 65% and 100% specificity, and its genotyping possibilities. The time taken is a significant drawback.
The Xpert MTB/RIF assay is now recommended by the World Health Organization (WHO) for detecting M. tuberculosis DNA. This assay is rapid and inexpensive, providing both bacillary detection and results on the sensitivity of the bacillus to rifampin, the most commonly used anti-TB drug. It is slowly becoming the first line of testing for TB worldwide.
While smear microscopy takes one day, compared to the Xpert MTB/RIF hours, its sensitivity is <60% vs.>90% with the latter. Detection rates are significantly enhanced in HIV-positive individuals, yielding 45% higher sensitivity and thus helping them begin treatment earlier. The testing for rifampin sensitivity allows for early initiation of therapy for multi-drug-resistant bacillus strains.
Whole-genome sequencing (WGS) and Next-generation sequencing (NGS) are sophisticated and expensive methods, are not yet extensively available, and are currently performed in specialized centers only. Tissue examination under the microscope to identify granulomatous changes and/or the presence of the bacilli are other techniques used to diagnose the infection.
Indirect supporting evidence includes findings from blood tests, including complete blood counts, C reactive protein and renal function tests, urinary lipoarabinomannan (LAM), imaging, and endoscopic techniques. While specific signs of TB have not been described, there are non-specific signs that strengthen the diagnosis when added to other clues.
These include, for example, granular opacities due to nephrocalcinosis, punctate calcification due to healed tuberculous granulomas, small hypoechoic masses in the kidneys due to granulomas, mucosal thickening of the involved ducts or calyces or ureters.
Management
Once diagnosed, urinary TB is treated with four drugs for two months, with two medications being continued for another four months. Some patients need more prolonged courses. If multi-drug resistant TB (MDR-TB) is identified, treatment using various other drugs could be required.
Common side effects vary with each drug, but in general, isoniazid can cause hepatitis and neuropathy; rifampin colors the urine red or reddish-orange and can cause joint pain; pyrazinamide can cause uric acid levels to rise, causing joint pain' and ethambutol may cause optic nerve toxicity. To manage these, liver function monitoring, pyridoxine supplementation to prevent neuropathy, and regular vision checks are mandatory.
Surgical correction may be required for strictures of the ureter, or hydronephrosis, by inserting stents or percutaneous nephrostomy.
If adequately treated, urinary TB responds well in 90% of patients. About 6% of patients may relapse after five years. A multidisciplinary approach is necessary to identify and treat the disease in its various forms and mitigate its adverse sequelae and complications as well as its management.
References
- Jha, S. K. et al. (2022). Genitourinary Tuberculosis. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557558/. Accessed on August 18, 2022.
- Muneer, A. et al. (2019). Urogenital Tuberculosis — Epidemiology, Pathogenesis and Clinical Features. Nature Reviews Urology. https://doi.org/10.1038/s41585-019-0228-9. Retrieved from https://www.nature.com/articles/s41585-019-0228-9. Accessed on August 18, 2022.
- Merchant, S. et al. (2013). Tuberculosis of the Genitourinary System-Urinary Tract Tuberculosis: Renal Tuberculosis-Part I. Indian Journal of Radiologic Imaging. https://doi.org/10.4103%2F0971-3026.113615. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3737618/
- Tuberculosis (2021). Retrieved from https://www.who.int/news-room/fact-sheets/detail/tuberculosis. Accessed on August 18, 2022.
- Covid-19 Deaths This Year Have Already Eclipsed 2020's Toll (2021). The Wall Street Journal.Retrieved from https://www.wsj.com/articles/covid-19-deaths-this-year-have-already-eclipsed-2020s-toll-11623350773?mod=hp_lead_pos1. Accessed on August 18, 2022.
- Altiparmak, M. R. et al. (2015). Urinary Tuberculosis: A Cohort Of 79 Adult Cases. Renal Failure. https://doi.org/10.3109/0886022X.2015.1057460. Retrieved from https://www.tandfonline.com/doi/full/10.3109/0886022X.2015.1057460. Accessed on August 18, 2022.
Further Reading
- UTI Symptoms
- UTI Diagnosis
- UTIs and the Immune Response
- What is TB?
Last Updated: Jun 7, 2023

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article